Restless nights can ruin your days. A sleep study may be able to help
Rick Bonow feels like a new man. His mood is more upbeat; he arrives at his job early and full of energy; he has started working out for the first time in years. His new energy can be traced back to one thing: a good night’s sleep—thanks to a night spent in a sleep lab.
For years, Bonow, 45, had been struggling with obstructive sleep apnea. At night, his breathing would become shallow or even stop. In sleep apnea, the tongue or tissues in the throat relax and obstruct a person’s airway. A person with sleep apnea may briefly stop breathing five to 30 times per hour—or more—during sleep.
Bonow knew something was wrong when he started nodding off at the wheel of his car. He was tired all the time, even though he thought he was getting plenty of sleep at night. As a laborer for the Village of McCook, where he cuts trees, plows snow and drives a truck, he knew that his tiredness was putting him—and others—at risk. “I was slow-witted. I couldn’t think fast,” he says. “Everything started lagging.”
Bonow visited a sleep lab for the first time in 2007 and received a diagnosis of obstructive sleep apnea. In the years that followed, he used a continuous positive airway pressure (CPAP) machine, which blows air into the nose through a mask, to control his symptoms, but his sleep was still suffering.
Recently, he heard about Inspire Therapy surgery at NorthShore University HealthSystem, in which a small, implanted system monitors and stimulates muscles to keep a person’s airway open while sleeping. He had the surgery last summer and now goes back to the sleep center to have adjustments made as needed.
A night at the sleep lab
Thomas Freedom, MD, program director of sleep medicine at NorthShore University HealthSystem, regularly sees patients like Bonow.
“For health, sleep is as important as diet and exercise,” Freedom says. Patients come to the sleep center saying that they aren’t sleeping well, can’t fall asleep, can’t stay asleep, wake up tired or feel fatigued throughout the day.
During a sleep study, a patient typically arrives at the sleep center after 8:30 p.m. and settles into a small room that resembles a bedroom, with a bed, TV and nightstand. A tech attaches sensors and electrodes to the patient for data collection and then lets him or her watch television or read before drifting off.
Once sleep sets in, staff members look at brain activity using an electroencephalogram (EEG), measure eye movements to determine various stages of sleep and evaluate muscle activity through a sensor placed on the chin. They also check for leg movement using electrodes on the shins, monitor oxygen levels using a sensor on the finger, and monitor breathing through sensors on the mouth and nose and belts around the chest and abdomen. The tests go on for a minimum of six hours before the patient awakens and leaves the next morning.
There are nearly 60 sleep disorders, Freedom says, but frequently the diagnosis is sleep apnea. The disorder is second only to insomnia, which is the inability to fall asleep or stay asleep.
The importance of sleep
Even with all of the data the sleep lab reveals, Freedom says that the science of sleep still has an air of mystery to it. There is much unknown. “With all the research that goes on and all of the information that we have, we really don’t know why, exactly, sleep is needed,” he says.
But physicians do know the adverse impact of not sleeping well.
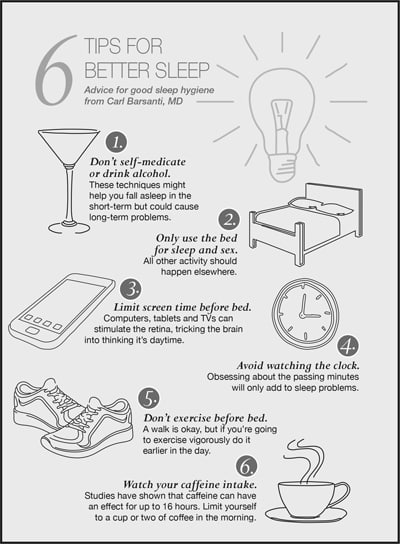
Carl Barsanti, MD, a pulmonary and sleep medicine specialist at Advocate Good Samaritan Hospital in Downers Grove, frequently works with patients suffering from sleep apnea and other breathing disorders. He says that tests in animals have shown that sleep is vital to health. “Extreme sleep deprivation can cause severe illness, immunologic deficiency and death in certain animal experiments,” he says.
Barsanti says that sleep apnea, in particular, can have long-term cardiovascular consequences if untreated. During sleep apnea, blood oxygen levels drop and blood pressure increases, which stresses the cardiovascular system. “It becomes a risk factor for heart disease, just like untreated high blood pressure, cigarette smoking, poorly controlled diabetes and high cholesterol.”
The impact of sleep deprivation can trickle into all areas of life, Barsanti adds. It can make a person feel cranky, tired and run down; work can suffer; it can increase the risk of motor vehicle accidents; it can impact friendships and relationships and even lead to sexual dysfunction and depression.
Barsanti and Freedom share the same advice: If you suspect you have a sleeping disorder, talk to your doctor about it. Treatment could transform your life, like it has for Bonow.
“It is absolutely great. I’m more awake. I think faster, and I feel stronger because I’m resting better,” Bonow says. “It’s unbelievable how it affected me.”