Telemedicine delivers remote healthcare on demand
By Karen Grimaldos
Pamela Ziegler doesn’t have time to get sick. That’s why when this busy working mom from Bartlett started sneezing, coughing and wheezing, she tolerated the bothersome symptoms for a week, hoping that they might go away on their own. When they didn’t, she went online to the DuPage Medical Group website and signed into her doctor’s patient portal to request an appointment.
What she discovered when she logged in to the site was a surprising new option that she didn’t know she had: a video visit.
She clicked and set one up. “I was a little nervous about not being able to do it correctly, but it was really easy,” Ziegler says. “I just didn’t have the energy to wait for an appointment and then drive out to the doctor’s office and back. I requested my video appointment online at about 5 o’clock and by 8:30 that evening, I was already talking to the doctor.”
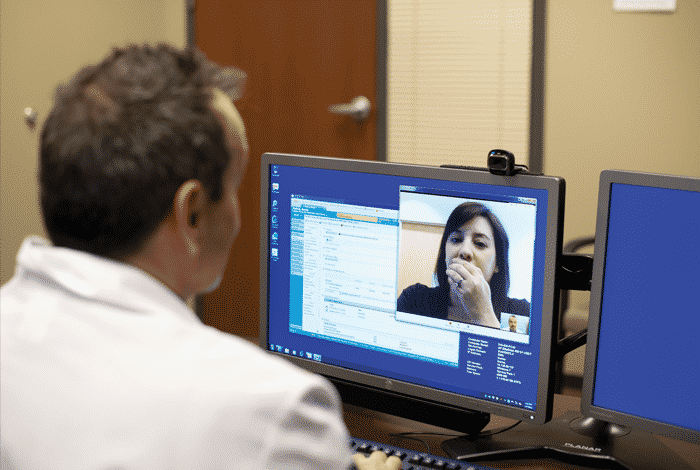
Ziegler used her home computer to Skype with a doctor who was in practice with her primary care physician. They were both able to see and hear each other during their e-visit, and the doctor had access to her file and records. Ziegler was diagnosed with a sinus infection, and the doctor also prescribed two prescriptions for her. Within a few days, she was feeling much better—no office visit required.
Welcome to telemedicine—a world of remote healthcare that includes all kinds of applications and patient services delivered via video conferencing, email, smart phones and other wireless tools and telecommunications technologies. More than half of all hospitals in the United States are currently using it in some form.
“Telemedicine is skyrocketing. It will double the number of patients [who] receive services in the next two years,” says Jonathan Linkous, CEO of the American Telemedicine Association in Washington, D.C. “It’s not only growing in the number of services that are being provided but also in the types of services.”
According to Linkous, telemedicine is currently being used for everything from remote monitoring of patients in intensive care units to accessing remote specialists for patients who are admitted to hospital emergency rooms.
Direct-to-patient video visits like Ziegler’s are also slowly starting to become more widely available. Because many insurance companies do not cover telemedicine services, the implementation of video visits has not yet become widespread.
Here in Chicago, the DuPage Medical Group, which has about 50 sites in the western suburbs, is leading the way when it comes to video visits. According to Maria McGowan, marketing director for DuPage Medical Group, as of this spring, they were the only medical group in the Chicagoland area to offer video visits to their patients.
Patients are charged $50 for their video visit and participate by using their mobile device or desktop computer with a web camera. Currently, primary care physicians that conduct video visits work out of a central location in DuPage County, which is equipped like one of their offices. The site includes two screens to allow access to the patient chart and to see the patient through a secure video connection during the visit.
“We don’t treat any severe or complicated conditions with video visits. Lots of the visits tend to be for respiratory [issues], rashes, back pain, anxiety or depression,” says Mark P. Nelson, MD, a family physician at DuPage Medical Group.
Most issues that are being dealt with during these visits do not require a physical exam, but doctors can capture images of a rash, for example, or observe whether a patient with back pain can stand up, bend down or twist.
“You can’t examine the patient, so you always have to remember that. If you’re not really clear on the situation from what you’re hearing from the patient, then that’s when you need to ask them to come in,” Nelson says.
At Advocate Christ Medical Center in Oak Lawn, telemedicine is not being used in outpatient settings but rather in the in-patient units and emergency department to treat behavioral health issues. This is the result of a recently launched proactive screening program by Advocate Health Care to detect undiagnosed and undertreated behavioral health conditions in select hospitals that have telemedicine capabilities.
“Because there is a great shortage of behavioral health providers, patients can go days without being evaluated in some hospitals, or sometimes they’re not evaluated at all,” says David Kemp, MD, a psychiatrist at Advocate Christ Medical Center. “Telemedicine offers patients immediate access to a clinician with expertise.”
The telemedicine equipment consists of a large monitor and camera that can be controlled remotely from the location where the psychiatrist is sitting. A nurse typically wheels a mobile cart with the equipment into the patient’s room and then places it in front of the patient to start the one-on-one session.
Although the hospital is using telemedicine for brief, short-term evaluation, diagnosis and treatment, the results can still be lifesaving. In one such recent case, an emergency room social worker at Advocate Trinity Hospital in Chicago administered a routine behavioral health screening to a patient, which indicated the presence of clinically significant depression or anxiety. The medical team was able to schedule a telemedicine session with a remote psychiatrist at Advocate Christ Medical Center to get the patient immediate help.
“We were able to intervene and pick up on suicidality,” Kemp says. “We were able to make a diagnosis of bipolar disorder and start that individual on medication. That suicidality risk would have been missed without the use of telemedicine technology.”
Kemp says there have been several cases where his team has identified suicidality risk in patients, and many of these individuals would never have even seen a psychiatrist if it were not for the telemedicine program. “Some of these patients were recommended to see a psychiatrist, but they never followed up, or there was too long of a wait to get an appointment, so they fell through the cracks.”
The option of telemedicine eliminates any of those obstacles of care.