The autonomous nervous system’s longest nerve runs from the brain into the gut, helping the body rest, relax, and digest
Fact checked by Jim Lacy
Have you heard of the vagus nerve? I certainly hadn’t — until my son, who has a host of food allergies and other health issues, experienced anaphylaxis this past spring.
After picking him up from school, I realized something wasn’t right. We headed to urgent care, and by the time we saw a doctor, my son was wheezing for air. Within three minutes of an epinephrine injection, he improved.
Prior to this, we’d seen a number of specialists to address his food allergies. In our hunt for answers, I’ve lost count of how many times my son has said his stomach hurts or “nothing tastes good.”
Eventually, an occupational therapist directed us to The Health Doctors, Ltd. in Warrenville. Unlike traditional chiropractors, this group also works on the vagus nerve to calm the body down, performing gentle adjustments to help the body heal itself.
I had no idea what that really meant.
What is the vagus nerve?
The vagus nerve, which runs like a super highway between the brain and gut, impacts virtually every body system, including sensory and motor functions. It’s involved in mood management, inflammation, digestion, heart rhythm, and respiration.
“The vagus nerve is known as the wandering nerve,” says John Zajecka, MD, professor of psychiatry at Rush University Medical Center.
The nerve travels from the brain down the spinal cord, through the neck, chest, stomach, and intestines. Along the way, it splits off into branches, controlling involuntary motor and sensory functions including heart rhythm and digestion.
“It is a key component for how we regulate what our body does,” says Naoum Issa, MD, PhD, section chief of clinical neurophysiology and director of epilepsy research at the University of Chicago Medicine.
The vagus nerve also impacts taste, the ability to swallow and speak, as well as skin and muscle sensations; it regulates mucus, saliva production, and urine output.
And it’s bidirectional. The left side goes up toward the brain. The right side descends into other organ systems that send signals to the digestive, cardiac, and respiratory systems. As the body’s main modulating nerve, it impacts a multitude of neurotransmitters, Zajecka says.
Jim Claussen, co-owner and chiropractor of The Health Doctors, Ltd., uses an automobile-related analogy to describe how the vagus nerve works.
If the sympathetic system, which manages the flight-fight-freeze response, is the gas pedal for our body, he says, the vagus nerve is the brakes.
For many people, especially kids, Claussen says, the gas pedal is stuck on accelerate. “It’s like driving a high-performance car with bicycle brakes. How efficient is that ride going to be? Not at all.”
This comes out as reactions that don’t match the situation, including seizures, constipation, and behavioral issues. The imbalance between parasympathetic and sympathetic nervous systems has become so great in this scenario that the person’s systems can’t perceive how to respond appropriately. “It’s not anybody’s fault. It’s just a wiring issue,” Claussen says.
Getting unstuck
People can get stuck after physical, chemical, or emotional stressors set the body into fight-or-flight mode, says Mouneesha Tatineni, a chiropractor at The Health Doctors.
Instead of recharging, the body is focused on surviving and getting through the day. Difficulty falling asleep or digesting food, or flare-ups in chronic illnesses like eczema can all be symptoms of the body stuck in fight-or-flight mode, Tatineni adds.
To try to reset the vagus nerve at home, Tatineni says people can try gargling, singing, humming, or chanting “Om.”
“All vibrate the back of the throat, which will vibrate the vagus nerve,” she says.
Chiropractic adjustments can help too, especially those that involve the patient holding their breath for an extended period and exhaling as the practitioner triggers different points on the body before performing adjustments.
Deep belly breathing also helps, as long as the exhale is longer than the inhale, Tatineni says because it stimulates the diaphragm muscle, through which the vagus nerve passes.
“All of this will get you out of that freeze mode and activate the brakes, which is the healing side of things,” she says.
Vagus nerve stimulation therapy
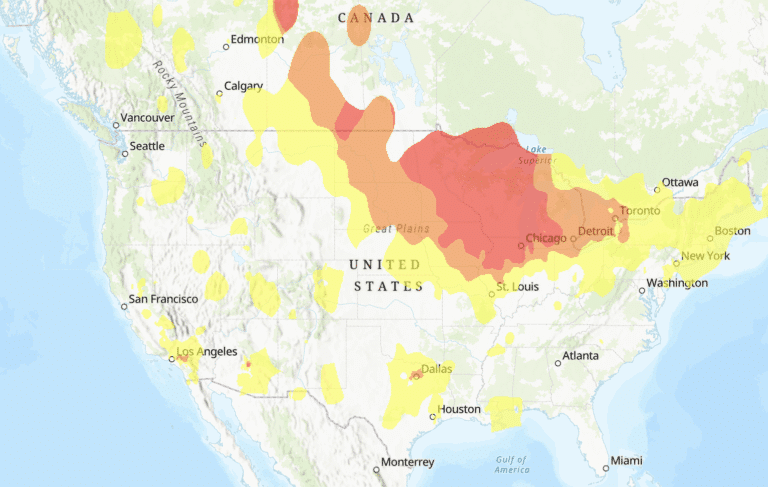
In recent decades, the FDA has approved vagus nerve stimulation (VNS) to treat patients for multiple health ailments including epilepsy, treatment-resident depression, and post-stroke motor rehabilitation. Through an implant, physicians are able to send impulses to the vagus nerve.
For people who struggle to use their hands and arms but have some function after a stroke, the device helps make new pathways in the brain, says Peter Warnke, MD, neurosurgeon and director of stereotactic and functional neurosurgery at UChicago Medicine. He was the first in the Midwest to perform the implantation for stroke rehabilitation in 2022.
The treatment activates deep brain structures, which are also involved in epilepsy and depression, Warnke says.
Epilepsy often develops after brain trauma because of a disconnection in the nerves. “Nerve cells are meant to be active,” Issa says. “If they don’t get the input because of disconnection from a tumor or trauma, they start to become hyperactive, trying to find inputs from other areas.”
That hyperactivity can create seizures, but vagus nerve stimulation acts as a pacemaker for the brain. “It’s providing excess activity that says to the nerves, ‘You’re doing something. You can calm down. You don’t have to have a seizure,’” Issa says.
The vagus nerve stimulator used for epilepsy and depression is a mini computer only slightly bigger than a credit card, embedded on the upper left side of the chest. Two wires go from the device and wrap around the left vagus nerve in the neck.
“For some, people it’s uncomfortable, but many people don’t mind it. Over time it reduces seizure frequency, and it improves your mood,” Issa says.
For that reason, the treatment can also help people with recurrent depression, who have failed four or more anti-depressant treatments, Zajecka says. It increases brain-derived neurotrophic factor (BDNF), a protein found in the brain. “It’s basically a brain fertilizer,” Zajecka says.
For our family, seeing a neurological-based chiropractor who works on the vagus nerve has made a huge difference, like a secret weapon for fighting stress and inflammatory reactions. My son’s symptoms ease if he’s having an allergic reaction. Besides reducing pain in his back and legs, his lymph nodes are less inflamed, and his tummy feels better.
Right now, I’ll take all the help I can get, to help him feel better.
Above photo: Peter Warnke, MD. Courtesy of UChicago Medicine
Originally published in the Spring/Summer 2025 print issue.

Dawn Reiss is a food-allergy mom and journalist. She loves swimming and traveling, learning new food hacks and getting off the beaten path.