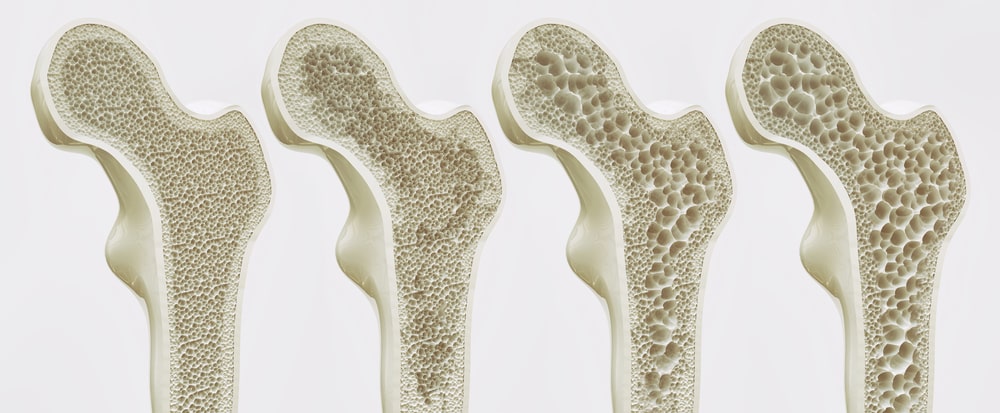
It’s all too easy to take our bones for granted. Day to day, they feel so strong and permanent, but in reality, our bones are alive and constantly changing. Their evolution is easy to overlook—until the day we realize how stooped our posture has become, or how easily our wrist fractured during a small and simple fall. These are just a few of the outward symptoms of a bone disease called osteoporosis.
Thinning of bone tissue and loss of bone density are the hallmarks of osteoporosis, which means “porous bones.” The condition makes bones fragile, brittle and susceptible to fractures, especially in the hip, spine and wrist. According to the National Osteoporosis Foundation, 10 million Americans—80 percent of whom are women—have osteoporosis; another 34 million have low bone mass and are therefore at risk for developing the disease. In fact, osteoporosis is a major health threat for a whopping 55 percent of Americans aged 50 and older.
The disease is of particular concern to the elderly, for whom fractures due to osteoporosis pose a significant health risk. About 1 in 10 men and 4 in 10 women over 50 will break a hip, spine or wrist, and shockingly, older women are at greater risk for death after a hip fracture than after breast cancer, says Dr. June McKoy, assistant professor of medicine and preventative medicine at Northwestern Memorial Hospital in Chicago. Studies have actually shown that approximately 24 percent of patients with hip fractures die within one year.
Detection and Prevention
Though osteoporosis’ painless and largely invisible progression has earned it the title of “the silent disease,” it can be detected early. A patient needs only a bone mineral density test (BMD), also called a DXA scan, which takes an image of the hip and spine. The test is painless and takes less than fifteen minutes.
“The bone density test is the gold standard for diagnosing osteoporosis and also for follow-up after treatment,” says Dr. Pauline Camacho, director of the Loyola University Health System Osteoporosis and Metabolic Bone Disease Center.
Medicare recommends—and covers—bone density tests for all postmenopausal women 65 and older. (The National Osteoporosis Foundation also recently recommended screenings for men older than 70, but that has not yet been translated into Medicare coverage.) However, Dr. Camacho screens women when they reach menopause, regardless of age, and private insurers usually cover the test. “A lot of patients may already have osteoporosis, so it’s good to act on it as soon as possible,” she explains. “It’s also good to get a baseline reading, since the first six to eight years after the cessation of menses have the fastest bone loss rate.”
Dr. Camacho also recommends screening for a deficiency in vitamin D, which is an issue for many Americans. The vitamin is crucial in helping the body to absorb calcium, so low levels are a well-known cause of bone loss. A doctor can prescribe the appropriate amount of supplemental vitamin D—which may be a better idea than baking in the sun, a strategy that’s surrounded by conflicting opinions.
“Dermatologists always recommend using sunscreen, which eliminates the skin’s pathway of getting vitamin D,” Dr. Camacho explains. “[On the other hand], endocrinologists recommend a couple of minutes of sun exposure a day without sunscreen. But as we get older, the skin’s ability to utilize the sun to make vitamin D decreases, so after a certain age, healthier people could spend 15 minutes in the sun.” She concludes, “If you take vitamin D pills, there is definitely no risk of getting skin cancer, and the conflict is resolved.”
Maintaining an appropriate level of vitamin D is just one of many lifestyle choices that can influence bone health—either positively or negatively. For example, both smoking and excessive alcohol use are linked to increased risk for osteoporosis. Smoking increases estrogen loss in women who are perimenopausal or postmenopausal and can result in a loss of bone density, Dr. McKoy says. And too much alcohol prevents your body from absorbing calcium properly, she adds.
Perhaps the greatest key to avoiding osteoporosis later in life is building strong bones at a young age. Why? Because women stop building bone mass in their 30s, Dr. Camacho says. Think of bone as a bank account where you deposit and withdraw calcium, Dr. McKoy says. During childhood and the teen years, new bone is added faster than old bone is removed. To maximize peak bone mass, when bones are at their strongest, children must get enough calcium, vitamin D and exercise. “Getting enough exercise and eating a calcium-rich diet is an investment in the future,” she says. Limiting soda is also important. “Often teens rely on the empty calories in soda to fill them up, and they do not get enough milk or calcium-fortified juice,” Dr. McKoy says.
Treatment and Future Directions
Sometimes, even the most conscientious efforts can’t ward off osteoporosis. Fortunately, researchers and physicians have recently debuted several advancements in the treatment of disease, particularly in the field of endocrinology.
Reclast, which was approved by the FDA in 2007, is a once-a-year treatment that slows bone breakdown and increases bone density. The patient receives an annual intravenous infusion of the drug (administered by a nurse or doctor) that takes about 15 minutes. Health professionals also administer a new drug called Prolia, introduced this past summer, which is injected twice a year.
Forteo is another drug that has shown positive results. “This is the only drug we have that actually forms new bone, but it is only approved for a patient to use for a period of two years,” Dr. Camacho says.
Osteoporosis has traditionally been treated with bisphosphonates, a class of drugs that includes Fosamax and Actonel. However, they do have drawbacks. Some patients have experienced spontaneous hip fractures that were not provoked by a traumatic event or have suffered from osteonecrosis, a breaking down of the jawbone. Thus, “It has become standard to give patients a brief rest from taking the drug every five years or so,” Dr. Camacho. “We are currently engaged in a study to find out how long this drug holiday should last.”
Though the risks are real, bisphosphonates remain very valuable. “These complications are very rare, and if we don’t give these drugs, we will see a lot of fractures,” Dr. Camacho says. “The risk of breaking a bone for a woman who has osteoporosis and is not being treated is very, very high. One needs to balance the benefits versus the risks.”
A drug regimen should always be supplemented with a daily routine of calcium-rich foods, calcium supplements and exercise (see sidebar.) Dr. Camacho recommends 30 minutes a day of weight-bearing exercise such as jogging, running or walking on a treadmill and lifting five- to 10-pound weights. Dr. McKoy stresses the importance of exercises that build strength, coordination and balance. Even better, women and men should adopt such a regimen long before an osteoporosis diagnosis ever enters the picture. Armed with proper education and fortified with a healthy diet, we can all enjoy a lifetime of strong, healthy bones.