Understanding the U.S. obesity epidemic
In October 2017, the Centers for Disease Control and Prevention (CDC) released its updated statistics on obesity in the United States. The numbers were troubling and confirmed what many have been seeing and predicting for decades: obesity is skyrocketing. Like a train that has run off track, we seem to be hurtling at rapid speed toward a clear disaster.
From 1971 to 2000, obesity rates among American adults more than doubled, from 14.5 percent to 30.9 percent, according to the CDC. As of 2016, the obesity rate had increased to 39.8 percent — a 29 percent jump in just under two decades and the highest rate in U.S. history.
If the epidemic isn’t curbed, by the year 2030 it is estimated that a shocking 51 percent of U.S. adults will be obese, according to a study published in the American Journal of Preventative Medicine.
Obesity affects both men and women relatively equally. The clearest lines of distinction appear to be set by ethnicity, with African-Americans and Hispanics experiencing higher rates of obesity than non-Hispanic Caucasians.
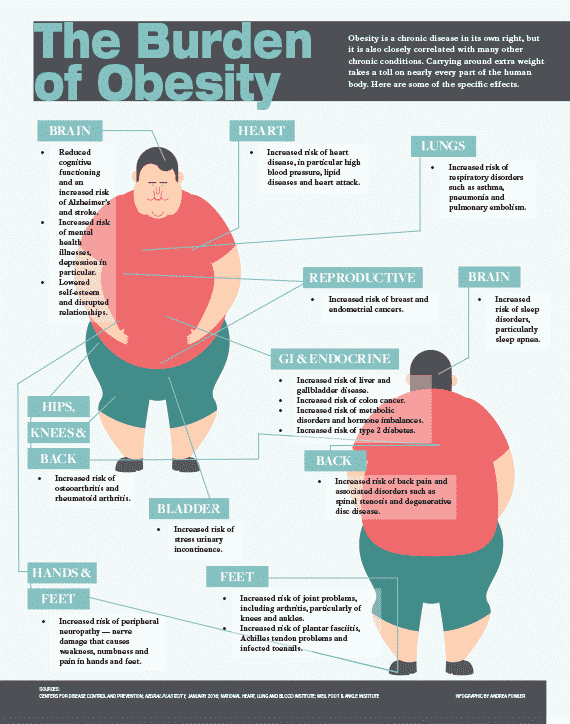
But statistics are just numbers, and obesity is, on every level, an extremely human problem. Unlike most other chronic illnesses, which have relatively clear causes and effects, how people become obese and stay obese, and the consequences of that extra weight, are multifactorial.
How do you solve a crisis with such various and complex human elements? With the health of our nation at stake, it’s a challenge that many in our country — and our city — have taken on in full force.
The roots of obesity
Keisha Isaacs first realized she was overweight when she was 8 years old. Her story is one that many others who struggle with their weight may recognize: a relentless pattern of emotional eating, spurred on in Isaacs’ case when her parents split up.
“I was always teased about being heavy,” says Isaacs, now 43. “There were two Keishas in my neighborhood, and I was known as ‘Big Keisha,’ ‘Fat Keisha.’”
The problems that cause obesity generally start in childhood. It’s when we develop many of our eating habits, and when we internalize the global and cultural influences around food that exist in our communities.
“I see very few people with any other problem except they just like to eat too much,” says Fred Tiesenga, MD, medical director of The Chicago Center for Bariatric Surgery & Medical Weight Loss at Westlake Hospital in Melrose Park. And most of them, he adds, are in denial about their weight, leading to a continued pattern of overeating that often doesn’t get addressed until the problem has gotten out of hand.
While eating too much might be the main culprit of obesity, Tiesenga is quick to clarify that the problem is much more complex than that. It’s the way people were taught to relate to food; the way their parents responded when they didn’t finish meals; the way people learned to use food as an escape. All of these things, Tiesenga says, need to be worked through when someone is trying to change their weight and their life.
Of course, there are other factors at play. There are medications and endocrine-related illnesses that can affect weight, though, Tiesenga says, those culprits are generally figured out pretty early.
Family ties
And then there are genetics. Isaacs says both of her parents were overweight, and her father is morbidly obese. The connection between weight and genetics is there, but it’s more tenuous than many would like to believe.
“You can’t blame just genetics,” says Christopher Chapman, MD, director of bariatric and metabolic endoscopy at UChicago Medicine. Genes do play a role, but it’s a complicated connection between multiple genes — not one single “fat” gene — and environmental factors.
“If you look at family groupings,” Chapman says, “someone with a family history of obesity is two to three times more likely to become obese.” Families don’t only share genes, they also share cultures and behaviors.
Part of the solution lies in teaching individuals, particularly parents, about healthy food options and portion sizes, and then supporting them in changing their habits, he says.
Then there’s the last piece of the obesity-causing puzzle: the brain. Whether obesity is a food addiction
is hotly debated. Both Tiesenga and Chapman note overlaps between the habits and neural reward processes around emotional and compulsive eating and those of substance abuse and addiction.
The lesson learned over decades of research is that the causes of obesity can’t be neatly compartmentalized.
The risks are both modifiable and incredibly difficult to control. They are interdimensional. They are physical, social and emotional.
And they are notoriously difficult to combat.
Weight-loss struggle
By her 40s, Isaacs weighed about 250 pounds at just over 5 feet tall and had spent more than 80 percent of her life either overweight or obese. There were periods where she dropped a few pounds — particularly during puberty and again in college when a doctor had her on the controversial weight loss drug phentermine — but most of those years were spent struggling with an uphill battle.
Isaacs says she would watch what she ate, but it wouldn’t make a difference. “I don’t go buy packs of cookies. Other people can sit and eat the whole pack and not gain a pound. I could look at two cookies and gain three pounds.”
Equally frustrating for Isaacs was the lack of difference made by exercise. At one point, she challenged herself to work out every day for 100 days. She completed her goal, but she didn’t lose much weight.
The more obese an individual is, the less likely they are to achieve sustainable weight loss without surgery. For those with clinical obesity, the odds of dropping to a normal weight without surgical intervention are 1 in 210 for men and 1 in 124 for women, according to a study published in the American Journal of Public Health. For people who are morbidly obese, the chance of achieving just a 5 percent weight reduction is 1 in 8 for men and 1 in 7 for women.
It’s a reset. I forget sometimes that I’m no longer big until I walk past a mirror.”
The problem is physiological. When dieting, your metabolism slows to match the decreased food intake. At this point, even if you’re starving yourself, you’re not going to lose much weight, Tiesenga says. This leads to discouragement and, often, a return to old eating habits.
The results of exercise for weight loss are similarly discouraging. A study published in Current Biology found that once you go above moderate activity levels, energy expenditures plateau. In other words: more work, the same results. While exercise still benefits your brain, body and overall health, it won’t necessarily do much for your waistline.
Successful surgeries
Weight loss surgeries, however, can make a lasting difference. A literature review published in JAMA Surgery in 2014 showed that bariatric surgery had sustained effects on weight loss, with continued loss of body mass index (BMI) five years after surgery.
While weight loss surgeries are by far the most effective means of treating obesity, only about 1 to 2 percent of those who are candidates for weight loss surgery actually get it, Tiesenga says. Fear of complications, financial limitations and misconceptions about the efficacy of the treatments all come into play. There’s also a pervasive stigma. Says Isaacs, “People think it’s cheating.”
The field of surgical weight loss innovation is an exciting one. Gone are the days when the only option available was gastric bypass surgery — a highly invasive and complicated restructuring of the gastrointestinal system. Today, there are quite a few highly effective, minimally invasive (endoscopic) procedures, with more on the horizon.
There’s the sleeve gastrectomy, available endoscopically and known more familiarly as gastric sleeve surgery, where the stomach is reduced in size so patients fill up faster. There are endoscopic weight loss balloons that reduce food capacity by taking up a portion of the stomach. There are gastric pacemakers, which use electric stimulation of the nervous system to decrease appetite, and malabsorptive tubes that reroute food directly out of the body through an exit site on a person’s anterior abdominal wall.
In 2016, Isaacs opted for sleeve gastrectomy and has since lost over 100 pounds. It’s a success, but one she credits only partly to the surgery. She works hard every day to follow a lifestyle that helps her maintain the loss, including eating a healthy diet and exercising regularly.

Surgery or no, sustained weight loss is impossible without necessary lifestyle changes, particularly a rejection of the processed, carbohydrate-heavy comfort foods that cause so many to gain weight in the first place, as well as the emotional relationship to that food.
“It’s a reset,” she says. “I forget sometimes that I’m no longer big until I walk past a mirror.”
The multidisciplinary approach
There’s also the way weight is talked about or, rather, not talked about. Even in primary care offices, individuals aren’t typically getting the encouragement they need to seek help.
“There’s been a taboo around telling patients they’re overweight, and I think, ‘Why? Why can’t we tell patients that they’re overweight? Why can’t we offer them a solution?’” Tiesenga says.
To help patients make the whole-life changes needed to lose weight, many hospitals employ a multidisciplinary team of dietitians, psychologists and behavioral therapists, along with medical staff, to give patients the tools they need to achieve real change.
“Meaningful, sustained weight loss requires comprehensive lifestyle modifications,” says David Davidson, MD, a cardiologist who heads NorthShore University HealthSystem’s Weight Loss Management Clinic.

“This includes the more obvious aspects like diet and exercise,” he says, “and also includes some things that are less well recognized as contributors to weight loss, like sleep, emotional eating and stress eating; fixing underlying medical problems like thyroid disorders; adjusting medications that can contribute to weight gain and in some cases using weight loss medications [along with] lifestyle changes.”
The key to helping patients lose weight, Davidson adds, is supporting them in widespread lifestyle changes, not just setting them up with short- term fixes.
Community tools
One way to help individuals lose weight is to give them better access to the healthy foods many of us take for granted.
At Chicago’s Presence Saints Mary and Elizabeth Medical Center, a $100,000 grant from the USDA has allowed for the introduction of the West Town Health Market, a twice-monthly event that subsidizes healthy foods for participants of the Supplemental Nutrition Assistance Program (SNAP), formerly the food stamp program.
In a study of more than 66,000 U.S. adults, it was found that those who live in food insecure areas are 32 percent more likely to be obese.
“In low-income areas you have options that might not be the healthiest but are the cheapest,” says Nick Groch, RDN, LDN, clinical nutrition manager at Presence Saints Mary and Elizabeth. “It’s a perpetuation of a lot of the food consumption factors that lead to high obesity rates.”
The West Town Health Market is a way to connect community members with the resources and education they need to eat healthier. Between 400 to 600 individuals regularly come to purchase fruits and vegetables, Groch says.
Such support is necessary to counter obesity. Very few can do it alone. While weight loss programs and surgeries can help in the battle of the bulge, nutrition and fitness follow- through is key.
“Just know that whatever way you go,” Isaacs says, “you’ve got to continue to do the work.”+