Holistic therapies and mind-body treatments can help with chronic pain
Kari Wagner was walking home from the park with her dog and 10-year-old son when she was thrust onto the asphalt. After that, she has only a few memories: lying in the street, being transported in an ambulance and being in the hospital.
A car had hit her from behind and sped off. The right side of her face took the brunt of the impact, causing a traumatic brain injury to her right frontal lobe. Fluid, swelling and clotting filled her forehead.
But what happened afterward became more gruesome for Wagner than the car accident. She experienced three months of continuous sinus infections, which led to sinus reconstruction surgery.
After surgery, “instead of getting better, the pain got worse and worse,” she says. Wagner visited a rotation of doctors and underwent several CT scans and MRIs. Specialists put laryngoscopes down her nose to inspect the problem.
“I finally ended up in the emergency room with a pain I had never felt in my life,” she says. She felt as if her face were being electrocuted and as if razor blades were cutting her lips. She was diagnosed with atypical facial pain and permanent nerve damage. “If I had a gun, I would have killed myself,” she says.
A neurologist later diagnosed Wagner with trigeminal neuralgia, a chronic condition that causes excruciating pain to run from your face to your brain. It’s commonly known as the suicide disease.
It was too painful for Wagner to eat. For months, she had a feeding tube. She could barely walk or let water hit her face in the shower. Brushing her teeth brought on unbearable pain.

She took a cocktail of opioids, as well as Trileptal, an anti-seizure medication that is also used for nerve pain. The more she took, the more she needed.
Desperate for answers and to get off the painkillers, she prayed for guidance and went to Minnesota’s Mayo Clinic and then to Northwestern Medicine’s Marianjoy Integrative Pain Treatment Center in Oakbrook Terrace. The alternative approaches she learned there finally cut her pain.
At Marianjoy, Wagner started using transcutaneous electrical nerve stimulation (TENS) to manage her pain. She learned about yoga, meditating with lavender oil behind her ears and wearing acupuncture earrings. She became a vegetarian and cut out sugar and caffeine. She started using essential oils like lemongrass, adding cinnamon (known for its anti-inflammatory properties) to her food and drinking a tea-like mixture made from hot water with fresh ginger and lemon juice to open the passages in her face.
Wagner also met Victor Foorsov, MD, a pain management specialist and physiatrist at Northwestern Medicine’s Marianjoy Rehabilitation Hospital in Wheaton, who opted to do a transnasal sphenopalatine ganglion block to relieve her pain. After the first treatment, the pain diminished so much that Wagner ran into the waiting room and kissed her husband for the first time in seven years.
“Everything happened so fast it was unbelievable,” she says.
Wagner usually goes for treatments once a month to help manage her chronic pain. “You begin to live in fear that the pain will be triggered,” she says. “Pain will never kill you, but you think it’s going to.”
And unfortunately, she’s not alone in her suffering.
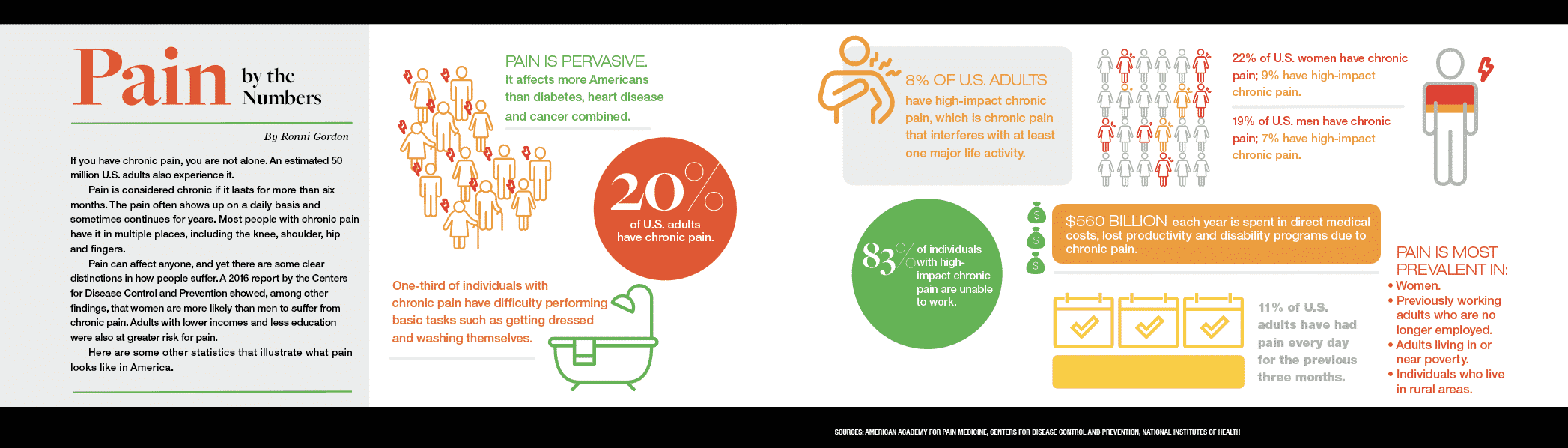
More than 20 percent of the U.S. adult population, approximately 50 million Americans, have chronic pain, according to the Centers for Disease Control and Prevention. Trying to find the most effective alternative treatments when you’re in pain and not sure where to go can be a time-consuming, trial-and-error-filled, expensive journey that usually isn’t covered by insurance.
Turning to alternative options
Many people turn to nontraditional healers if their problems are getting worse and they don’t want the two typical options: surgery or long-term usage of pain medicine.
Alternative medicine looks holistically at how body systems are interconnected instead of looking at ailments such as migraines, back pain and digestive complaints in isolation.
“In whole-body systems of medicine, like traditional East Asian, Ayurveda and homeopathy, we look at all of those problems as branches that have one root cause or two root causes,” says C. Leslie Smith, MD, director of integrative medicine and culinary medicine at the Southern Illinois University School of Medicine. “And then you treat the branches, but you also treat the root cause. People get better because you’re fixing the underlying issue as well as the symptoms.”
Smith personally understands. She was 14 months away from graduating from surgery residency when she developed radial tunnel syndrome, a repetitive stress injury that left her right hand paralyzed. It completely changed her trajectory and medical focus on alternative methods.
Her experience is the reason Smith founded the Chicago Healing Center in Uptown in 2012, which offers acupuncture, medicinal herbs, cupping, moxibustion, energy healing, nutritional counseling, medical lasers and osteopathic manipulation.
There’s a bias that alternative medicine is not evidence-based, Smith says, even though various cultures have used these techniques for thousands of years.
One example is Ayurvedic medicine, a whole-body healing system based on the five elements — air, fire, earth, space and water — which creates a mind-body framework that guides our physical, emotional and mental makeup.
“Ayurveda has been used for thousands of years to treat abdominal pain,” Smith says. “So you don’t really need a randomized controlled trial when you have 5,000 years’ worth of clinical trials showing it works.”
The mind-body connection
Even though chronic pain can manifest itself in very real and physical manners, its triggers and true root causes can be complicated.

Some people can develop central sensitization, in which nonpainful stimuli evoke pain. For example, a migraine sufferer might not be able to wear a hat or put their hair in a ponytail because their nervous system is on overdrive, says Merle Diamond, MD, managing director of Diamond Headache Clinic.
“Chronic pain is a very complicated process. It doesn’t have to just deal with a person’s injury or event, but a person’s emotional response to that event,” Diamond says.
Trying to break the cycle of heightened sensitivity to pain can feel like a daunting, impossible task.
That’s why John Gribbin, Erich Luedtke and Laura Seago launched Chicago-based Curable, an app for chronic pain. Each of the founders suffered from chronic pain including migraines, sciatica, lower back, knee and hand pain. The app uses a chatbot to help users through pain education, breathing, meditation, cognitive behavioral therapy and writing exercises to redirect pain pathways and retrain the brain.
“It’s the brain-body connection,” says Gribbin, CEO of Curable. “For many, it’s more than just the act of meditating for 20 minutes a day that’s going to get you better. … When people can remain positive and instill hope in each other it is very powerful, and we see that they have a higher likelihood of getting better.”
John Stracks, MD, an integrative physician in Chicago and Northbrook and an assistant clinical professor of family medicine at Northwestern University, has emphasized the connection between mind and body since he started practicing medicine. He joined Curable’s scientific advisory board because of his longstanding work with patients who weren’t getting better via more traditional methodologies.
“What happens in our life comes out in our bodies,” says Stracks, whose practice focuses on mind-body disorders such as tension myositis syndrome (TMS), in which nerve pain, back pain, migraines and other chronic issues are caused by inner stress. “Conventional treatments don’t work for a lot of people. Many people have taken medications, had surgery or gone through physical therapy and haven’t gotten much better.”
“There’s a huge trauma-pain cycle,” Stracks says. “To treat chronic pain effectively, you have to treat both the brain and the body. You can’t just do one or the other.”
Balancing mind and body
Some chronic pain sufferers turn to energy work, which seeks to facilitate the flow of energy to help balance the body and mind and promote health and healing.
“The non-physical affects the physical,” says Shweta Shyamani, an alternative medicine practitioner who sees patients at the Chicago Healing Center and through her private practice, Personal Point of Power.

Like salivating in anticipation of eating a favorite food, a pain sufferer may anticipate pain before the actual act happens. Changing the nervous system to send different signals to the body shifts the mind-body connection.
“We have various energy systems that hold information about our body that work very closely with the nervous system, which influences every function of our body,” Shyamani says.
That’s why Shyamani is quick to tell patients she is not treating the symptoms, like irritable bowel syndrome, but finding the energy systems that contribute to that part of the body to change the signal.
“Science has shown us it is the environment that influences the cells,” Shyamani says. “The environment consists of things such as our nutrition and the quality of thoughts we have. Thoughts are packets of mental energy, and stressful thoughts send a signal different from peaceful ones. We convey new messaging to our physical selves by changing our energy.”
Changing the echo chamber
Finding new patterns is the reason Cheryl Hurst, PsyD, a health psychologist and yoga therapist in the Loop, began combining yoga therapy with psychotherapy.
“Psychotherapy isn’t enough for people with chronic pain,” Hurst says. “Patients tell me, ‘Talking about dealing with my pain just stirs the pot. I need to know what I can do about it and try approaches that work.’”
“Chronic pain is like an echo chamber where our own recoiling and cringing at the pain tends to reverberate throughout our nervous system, creating more pain,” Hurst says. “The pain and our response to it wears us down. If we don’t change the pattern through our awareness, actions and breath, the pattern doesn’t ease up on its own.”
“Even when we are physically doing better, sensory and mental conditioning often ties us to past patterns,” she says. “We need to teach ourselves to detach from the painful experience, the same way you detach from your thoughts during meditation. Thoughts still come up, but the idea is to not react to the thoughts, but just observe them. Then we can learn new skills to address the original pain source.”
That’s where yoga comes in to align the body and break the cycle. She recommends taking slow breaths with longer exhalations and repeating a positive mantra such as, “I can make a difference by actively regulating my own experience.”
“To start, be quiet and present with your own experience,” Hurst says. “It doesn’t happen very often, because usually we are too busy reacting.”
Food as medicine
To tackle pain, it’s also important to review your nutritional intake. For centuries, food has been used as medicine and has been the basis of pharmaceuticals.
Turmeric, a golden-colored spice from the ginger family, may help with pain due to its anti-inflammatory compound, curcumin.
“Turmeric deflates the inflammatory response,” says Michelle Wesely, DC, a certified functional medicine practitioner and chiropractor at Wesely Family Chiropractic in Glen Ellyn. “It downregulates NF-kappa B activation, a protein that controls the transcription of DNA. If it gets out of control, it can lead to chronic inflammatory conditions such as allergies, diabetes, muscular sclerosis and arthritis.”
Turmeric may reduce fatigue, depression and anxiety, Wesely says, because of its ability to cross the blood-brain barrier and protect the brain from inflammation. It also may reduce insulin resistance because curcumin may improve the function of beta cells that make insulin in the pancreas.
It’s important to couple alternative methods with self-care, says Northbrook clinical psychologist Sarah Allen, PhD.
“You’ve got to meet some of your own needs before you have the ability to look after everybody else,” Allen says. “Have your partner take over some things to get the support you need, so you don’t keep doing things that create flare-ups.”
For many people, the traditional medical approach is not sufficient, which is why once-alternative treatments are becoming more mainstream.
“Alternative approaches have a more holistic approach because they look at everything that is going on for a person,” Allen says. “That’s important because there’s always an emotional component to pain.”

Ellen Ryan is an award-winning writer/editor specializing in profiles, Q&As, and case studies; consumer health; education and career change, business; and grammatical near-perfectionism. (Nobody’s perfect.)