When chronic pain strikes, depression and anxiety can follow
Chronic pain is more than a physical problem.
Those who suffer from long-term pain often experience emotional and psychological aspects as well, particularly depression and anxiety. Add to that potential anger, frustration, hopelessness, fear and jealousy, and the emotional symptoms of chronic pain can quickly become overwhelming.
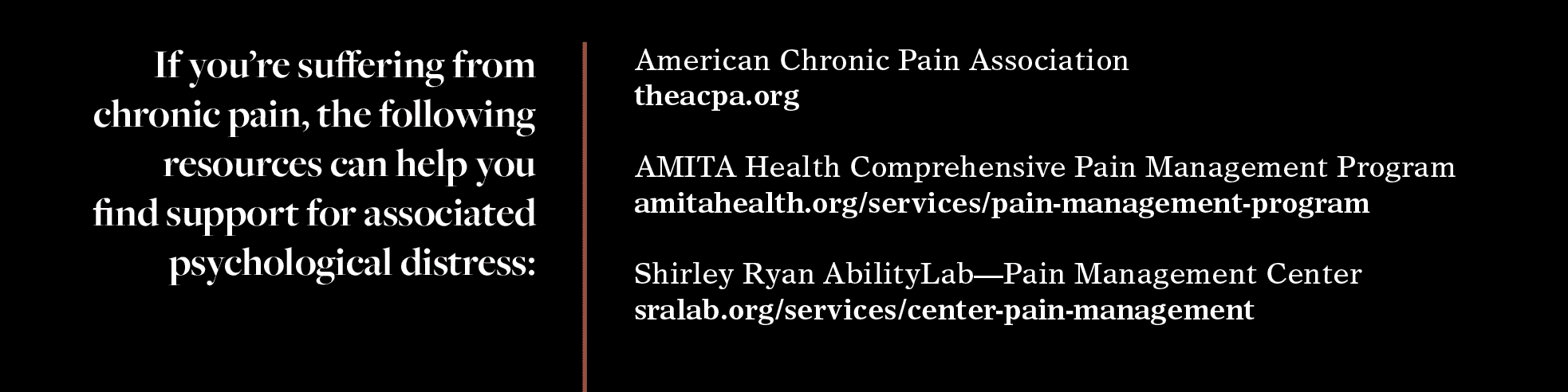
It’s critical to recognize the mental health aspects of pain early in a patient’s experience, says Konstantinos Kostas, PhD, director of health psychology services at AMITA Health.
“If depression and anxiety are not identified and treated shortly after a person is diagnosed with chronic pain, their quality of life can worsen,” he says. “[Patients] believe that their pain is behind most of their distress, when in fact it’s usually a combination of their pain and their emotional response to it that’s causing their distress.”
Emotional responses are closely associated with chronic pain. “The regions of the brain that encode pain also encode emotions,” says Diane Amstutz, PhD, a pediatric psychologist at the Pain Management Center at the Shirley Ryan Ability Lab.
A multidisciplinary approach can help counter depression, anxiety and other mental health issues associated with pain, says Ankur Dave, MD, a pain management specialist with AMITA Health. “This includes cognitive behavioral therapy, mind-body relaxation techniques, exercise therapy and, for some patients, the inclusion of medical management, including medications and interventions,” he says. “These treatments are first-line options for chronic pain. Data suggests that using these modalities together has the best results.”
Sarah, 24, a Chicago resident who requested that her last name not be used, has suffered from chronic pain for several years. She gets through her day with meditation, visualization and the Alexander Technique, a mind-body method that works by promoting alterations to posture and movement.
Sarah deploys strategies as needed, even while working or socializing. “I constantly try different tactics. I use an app. I meditate every morning,” she says. “I try to focus on my breath and be mindful with pain — to really feel it, but not judge it.”
Isolation is another burden for chronic pain patients. “Life shrinks up and people withdraw from physical and social activities,” Amstutz says.
Sarah has experienced this social withdrawal firsthand. “It becomes easier to be on my own because I don’t have to guard what I am going through,” she says. “If I’m with someone, I want to enjoy their company. But if I’m in extreme pain, I’ll find I’m getting more irritated because I want to attend to the pain. It’s hard for my family and friends to understand why I do not want to do certain things.”
Managing the physical and emotional aspects of chronic pain is challenging. But it can spur individuals to make positive changes in their lives. It “encourages people to examine their priorities and make changes that might be important to them,” Kostas says.
Sarah, too, sees a silver lining to the difficult emotional experience of pain. “I have what I think is a purpose to get better myself and then to help as many others as I can,” she says. She also appreciates the importance of her support system of family and close friends. “Some people don’t have that. I’m really lucky.”

Ellen Ryan is an award-winning writer/editor specializing in profiles, Q&As, and case studies; consumer health; education and career change, business; and grammatical near-perfectionism. (Nobody’s perfect.)












