Texas has sent more than 34,000 asylum seekers to Chicago since September 2022. Here’s a look at how local organizations have been responding to migrants’ health needs since the humanitarian crisis began.
Anna was 34 weeks pregnant when she arrived in Chicago. She’d boarded a bus in Texas, which dropped her off in the U.S.’s third-largest city 24 hours later. Not long after that, she ended up in a local emergency room.
Hospital staff contacted Erie Family Health Centers, a clinic that works with medically underresourced communities, to follow up with Anna (name changed for privacy) after the hospital discharged her. However, with no cell phone, no permanent address, and no transportation, step one for Erie’s certified nurse midwives was to locate her, says Kate Birdwell, associate director of communications at Erie Family Health Centers.
Tracking down an asylum seeker in one of the city’s many shelters can be a guessing game — and it happens frequently.
Anna ended up making contact first. Once she had secured a cellphone, she called a midwife at Erie Family Health Centers. She said that she was on a bus, being moved to a shelter in an unknown part of the city. Yet, she stayed with Erie Family Health Centers, taking multiple city buses, with her toddler in tow, to her weekly prenatal exams.
Anna delivered a healthy baby, but the difficulties she experienced accessing healthcare is widespread among Chicago’s new arrivals.
Since August of 2022, the City of Chicago reports that buses and planes from Texas have brought more than 34,800 people seeking asylum to Chicago. The people are dropped off unannounced, with no advanced warning or coordination between states to ensure the people receive shelter and care.
“Our biggest challenge is in continuing to adapt to meet the healthcare needs of an under-resourced population that is rapidly increasing in size,” says Jacob W. Martin, public information officer with the Chicago Department of Public Health (CDPH).
New arrivals undergo health screenings for acute illness, infectious disease, and existing medical conditions when they enter Chicago shelters. Screenings include Covid-19, tuberculosis, pregnancy, and more. Next, they are scheduled for a medical checkup at Cook County Health’s Belmont Craigin clinic, and if needed, they receive routine and seasonal vaccines.
CDPH also offers periodic vaccine events at new arrival shelters, with vaccines for influenza, Covid-19, and varicella (chickenpox). Since November, the department has held more than 50 events at 15 shelters.
Shelter staff coordinate further medical exams with Cook County Health, which opened a clinic in Belmont Cragin exclusively to serve this population and provide them a full-time medical home, Martin says. According to CDPH, case managers in shelters “are trained to connect residents to emergency services when necessary, to ensure that emergent illnesses are promptly detected and treated.”
Within the city’s 27 new arrival shelters, CDPH funds federally qualified health centers (FQHCs), and works with more than 10 other providers — including Heartland Alliance, Lawndale Christian Health Center, and University of Illinois at Chicago — to offer on-site care. The teams visit each shelter at least once a week to provide screenings, infection prevention, and behavioral health services, Martin says.
Still, the City of Chicago has struggled to provide essential medical care to the unprecedented number of asylum seekers, leading outside organizations to step in and fill the gap.

The Mobile Migrant Health Team began to address the care gap at police districts, which initially were the temporary landing zones for new arrivals, says Sara Cooper, a fourth year medical student at UIC, and co-founder and associate director of the Mobile Migrant Health Team.
From April to December of 2023, Cooper and a team of 80 volunteer medical providers — medical students, nurses, physicians assistants, and physicians — screened 8,951 people and provided additional triage and treatment to 2,134 individuals. “This migrant population has had no access to even the most basic of healthcare essentials after having endured physically and emotionally treacherous journeys,” she says.
The current surge in asylum seekers is coming primarily from Venezuela; however, there are also individuals from other Central and South American countries, Afghanistan, and China. People have traveled thousands of miles by foot, fleeing extreme poverty, and political and economic upheaval. From Mexico, they cross the border and enter the U.S.’s overtaxed immigration and asylum system, straining to handle the growing need.
In a new country, facing language, financial, and systemic barriers, accessing healthcare is a daunting task. This is especially true for those with pressing medical needs.
“A recurring issue we encounter is that of Border Patrol officials confiscating inhalers or prescription medications and then not offering an opportunity for a provider to reassess them,” Cooper says. “We have cared for many children who had anti-seizure medications confiscated and were at risk of seizing again were it not for our providers on-site to provide care. We saw similar situations for chronic conditions like hypertension or diabetes exacerbated by being without their meds.”
The death in December of 5-year-old Jean Carlos Martinez Rivero at a new arrivals shelter at Cermak Road and Halsted Street put newly arrived migrants’ plight into stark relief. While the cause of the medical emergency that led to his death remains under investigation, the tragedy highlights the real human cost of failing to identify and treat the most vulnerable.
Chicago shelters are currently housing more than 14,000 migrants, who report crowded conditions, suboptimal heating, and poor-quality food.
Starting in March of last year through December, Chicago Street Medicine volunteers coordinated with the city to provide essential care for new arrivals at police stations who were awaiting shelter placement. “The most prevalent health issues we encounter are wound care for injuries sustained during the journey, dehydration, asthma, chronic pain, and upper respiratory and gastrointestinal infections that are related to staying in close quarters,” says Reba Abraham, vice president of the Chicago Street Medicine non-profit board.
Once people receive shelter placement, outside healthcare providers have not been allowed access to continue serving them. However, the city has launched a survey for healthcare organizations interested in providing medical resources to new arrivals. More than 12 volunteer organizations have applied, Martin says.
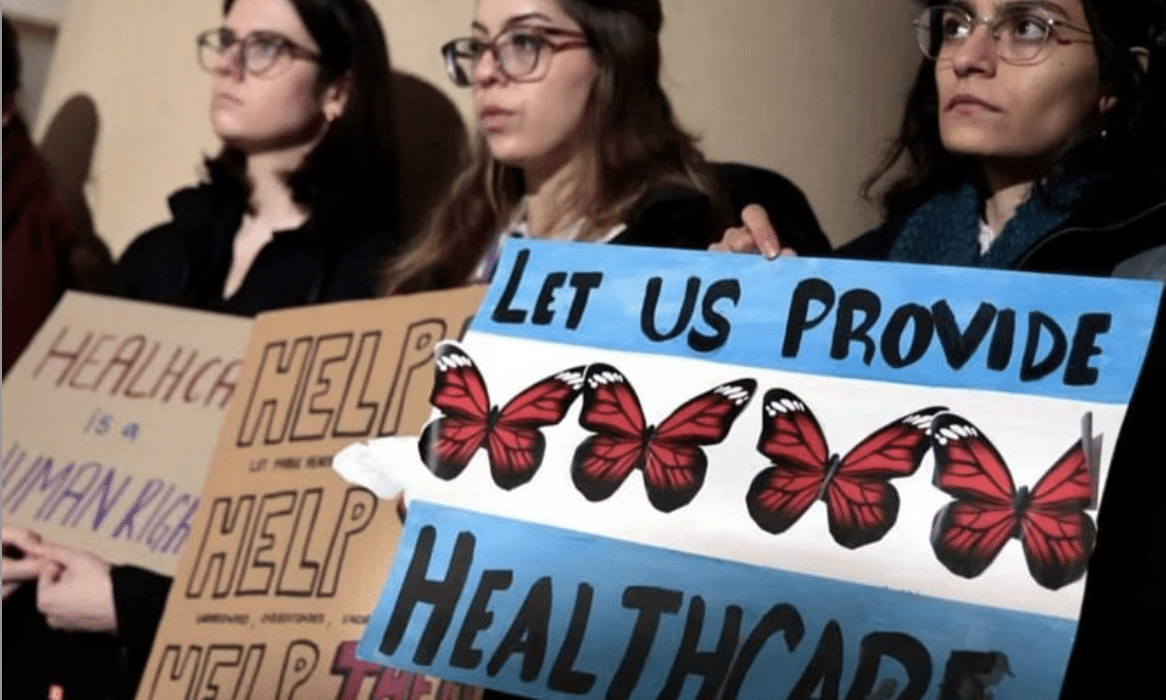
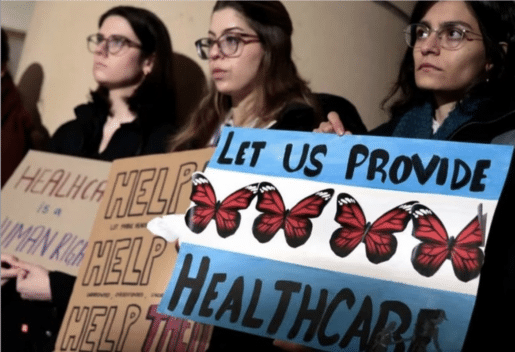
“At the moment, we are petitioning the mayor and city officials to be allowed inside city-run shelters to continue our work in triaging and helping provide preventative care,” Cooper says. “Gaining shelter access would be a way for the city to employ resources already at their disposal, and we are ready and waiting to continue caring for this population that means so much to us.”
She adds that CDPH Commissioner Olusimbo Ige, MD, recently gave Mobile Migrant Healthcare Team access to the landing zone. Chicago Transit Authority warming buses line up at this designated area, where the city tries to funnel the most recent arrivals as well as people who have to leave their shelter due to a city-imposed 60-day term limit.
“There is minimal food and basics provided there, and from what we have seen, minimal on-site healthcare,” Cooper says.
As complex healthcare needs of newly arrived migrants strain an unprepared healthcare system, volunteer medical professionals are leading the way in keeping the newest Chicagoans healthy.
Ways to Help Chicago’s Humanitarian Crisis:
- Join the Medical Reserve Corps.
- Donate season-appropriate clothing at Pilsen Food Pantry
- Fund the work of MMHT, Chicago Street Medicine, Erie Family Health Centers, and other crisis response medical organizations
- Deliver gently used winter coats to One Warm Coat
- Donate items off the Instituto Del Progresso Latino’s wishlist
- Check with the public schools in your area to see types of support they need