Floaters and flashing lights? It could be a retinal detachment
Christmas 2006 is a day I’ll never forget. My husband and I braved frigid temperatures to walk to a friend’s home. During dinner, a fly entered my field of vision. I swatted it away several times before realizing that I was the only person who could see it. From there, I saw other visions: what appeared to be beach balls bouncing in the corner, strange lights and so forth. But the next day was packed with work and family obligations, so I ignored these odd symptoms and carried on.
A day or two later, things were too pronounced to be ignored. By now, I had a line across my vision in my left eye, with no visibility beneath it. I called my father, who demanded that I go straight to the emergency room.
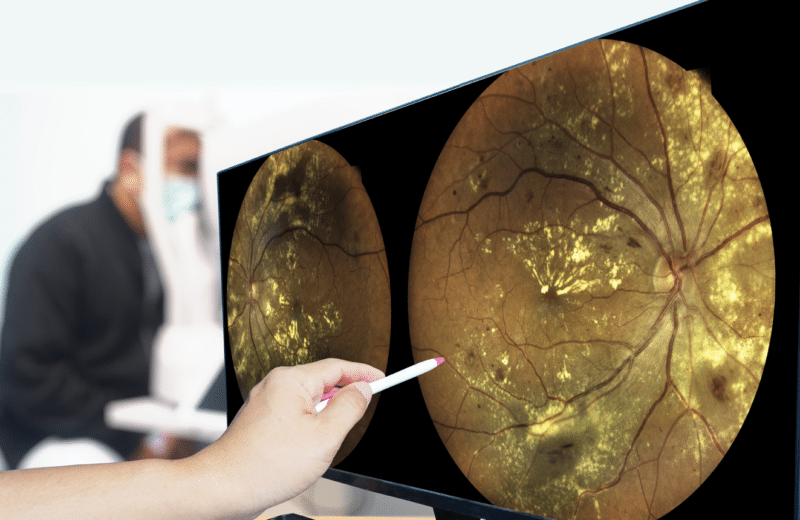
The ER resident quickly dispatched me upstairs to the ophthalmology department, where I met several doctors who talked and conferred and held up fingers that I couldn’t see. At last, I was informed of my diagnosis: retinal detachment with two additional tears.
What is the retina and what does it do?
The retina is a thin layer of tissue that covers the back of the eye. “The eye works like a camera, and the retina lines the back wall like film,” explains Mathew MacCumber, MD, PhD, a retina surgeon at Illinois Retina Associates and a professor at Rush University Medical Center.
The retina takes in light and sends the signals up the chain of command until they reach specialized nerve cells, which forward them via the optic nerve to the brain. The brain then decodes them into images.
Between the lens and the retina lies a gel called the vitreous. As people age, the vitreous liquefies and eventually, usually around middle age, it pulls away from the back of the eye. It can take the retina down with it, causing a tear, which can progress into a retinal detachment. A study published in 2010 in the British Journal of Ophthalmology found that the incidence of retinal detachment may be as high as 17.9 per 100,000 people.
High-risk patients should be aware of the symptoms — flashes of light, shade or shadows across the vision.
“Most tears begin with the vitreous pulling away,” says Manjot Gill, MD, associate professor of ophthalmology and director of vitreoretinal fellowships at Northwestern University Feinberg School of Medicine, who treated my detachment. “Vitreous fluid may pass through the break and can lead to a retinal detachment.”
The most common risk factors for retinal detachments are aging, family history and nearsightedness. People with high degrees of myopia (-8 or higher) are at higher risk. Retinal detachments can also happen after eye trauma or cataract surgery.
Anyone at risk for retinal detachment should be cautious and should know the signs, Gill says.
“High-risk patients should be aware of the symptoms — flashes of light, shade or shadows across the vision — and if they see them, they should visit an ophthalmologist immediately,” Gill warns. “Retinal detachments that are not treated promptly can cause loss of vision.”
Fixing tears and detachments
Retinal tears need to be sealed with a laser or cryopexy freeze treatment to secure the retina to the eye wall. For detachments, surgery is often needed to put the retina back in its proper position. The three main treatments for a detachment are pneumatic retinopexy, vitrectomy and scleral buckle.
1. Pneumatic retinopexy
This treatment involves injecting a small gas bubble into the area where the vitreous normally resides. The bubble helps push the tear against the eye wall, preventing further fluid from accumulating behind the retina. A laser or freezing therapy is also done to repair the break and help secure it. The bubble will eventually be absorbed. After this treatment, patients might be required to hold their head in a certain position, usually pointed downward, for a few days. This positioning helps the bubble push the retina back into place.
2. Vitrectomy
A vitrectomy needs to be done in an operating room. The doctor first removes the vitreous and any tissue that may be pulling on the retina through tiny incisions in the eye, and then fills the cavity with air, gas or silicone oil to help flatten the retina. As the eye heals, it makes fluid that gradually replaces the gas. Patients are often required to position themselves face down for two weeks following this procedure.
3. Scleral buckle
The scleral buckle is a silicone material that goes around the eye. In this surgery, the doctor sews a silicone band to the white of the eye (the sclera) over the affected area or areas. This indents the wall of the eye, relieving some of the forces that caused the retinal detachment. Once in place, the scleral buckle does not interfere with vision and is normally imperceptible to the wearer. Sometimes vitrectomy and scleral buckle are done at the same time.
One almost inevitable result of a vitrectomy is cataracts, which is a clouding of the eye’s lens. While cataract surgery is extremely common and becomes more likely as one ages, patients who have had vitrectomy surgery are likely to need it much sooner in their affected eye.
Because retinal tears and detachment do not cause pain or discomfort, it might be tempting to wait it out, as I did. But it’s important to see an eye doctor right away if anything strange comes across your field of vision, including flashing lights and floaters, say Gill and MacCumber.
And if you see flies and beach balls in the dead of winter, act quickly. Any significant changes in vision need to be evaluated immediately.