Polycystic ovary syndrome’s far-ranging impacts on women’s health
Back in 2013, Danni Allen, a native of Mundelein, shed 121 pounds and was crowned winner of NBC’s popular reality show, America’s Biggest Loser. Determined to keep the weight off, Allen maintained a lifestyle that included a healthy diet and plenty of exercise.
Yet in 2016, Allen noticed that the number on the scale started creeping up despite her commitment to health. She’d been previously diagnosed with endometriosis — a disorder that involves uterine tissue growing outside of the uterus — but she wanted a definitive reason for her unexplained weight gain and malaise. Allen wasn’t about to let all of her hard work fade into memory.
A revised diagnosis brought clarity. It turns out that Allen didn’t have endometriosis at all. She was diagnosed with polycystic ovary syndrome or PCOS. “I thought, ‘What the heck is PCOS?’” Allen says. “I’d never heard of it.”
Although it is called polycystic ovary syndrome, the disorder has nothing to do with cysts. Instead, what look like cysts in medical imaging are actually small, immature ovarian follicles. Follicles typically contain egg cells, and they release these cells during ovulation. For women with PCOS, abnormal hormone levels keep the follicles from maturing and releasing egg cells.
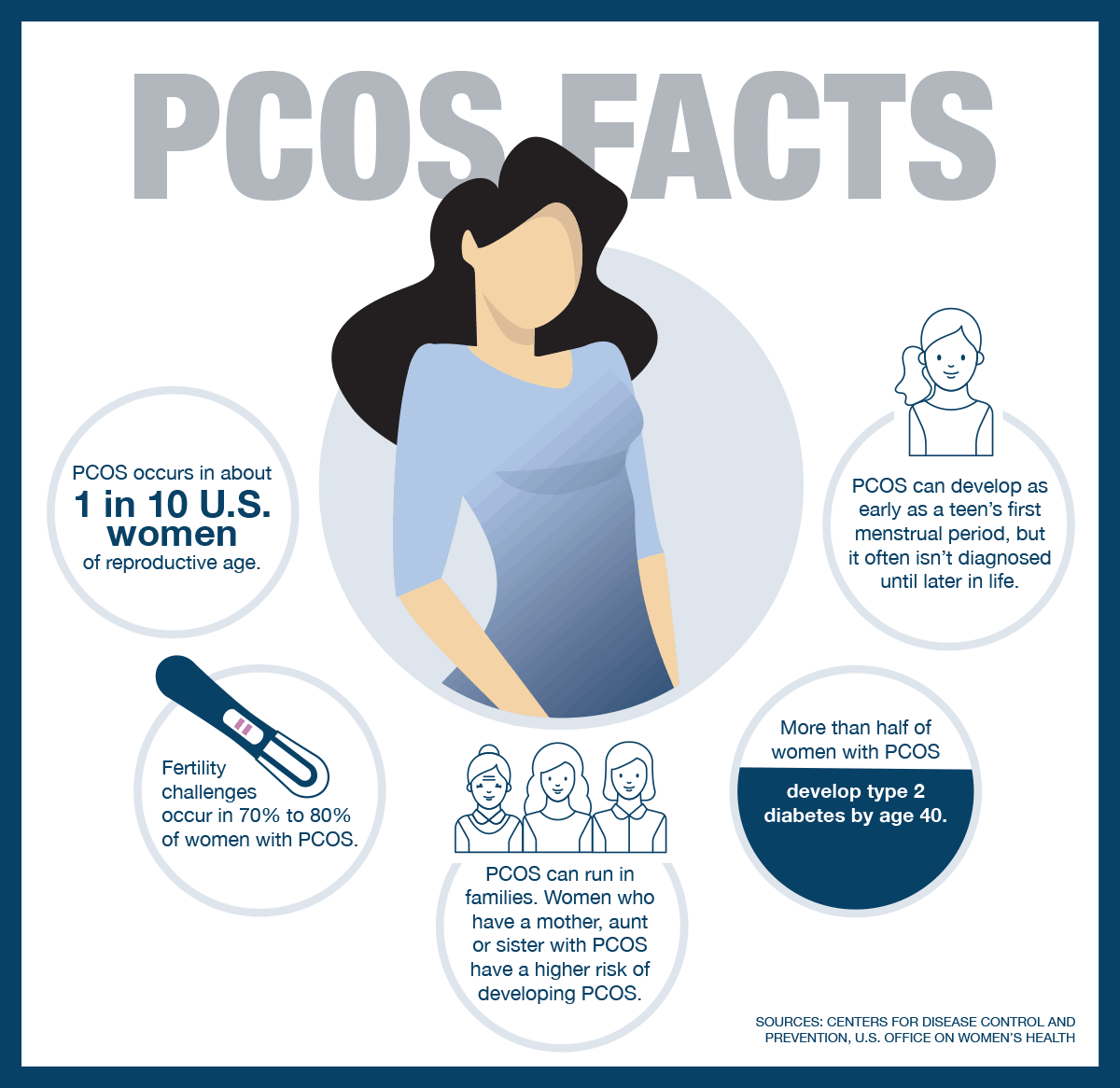
Allen had just joined the roughly 1 in 10 women of childbearing age diagnosed with this hormonal imbalance disorder. PCOS has wide-reaching effects. Besides irregular periods, it can cause excess body hair growth, weight gain and fertility challenges.
Roughly 5 million women of reproductive age in the U.S. live with PCOS, according to the Centers for Disease Control and Prevention. In addition to pain from enlarged ovaries, women with PCOS can find the emotional challenges of excessive hair growth and weight gain demoralizing. Women can also develop insulin resistance, which often goes hand-in-hand with weight gain.
Long road to diagnosis
Receiving a diagnosis for PCOS is one thing. But finding that diagnosis can be a much longer road.
“The average woman goes through [multiple] doctors until they finally find one who can diagnose the problem and help the patient take care of themselves,” says Frank González, MD, a reproductive endocrinologist at UI Health and a globally recognized expert on PCOS.
PCOS is commonly misdiagnosed as other disorders of the reproductive system. That’s because each PCOS case differs slightly. Some of the diagnosis challenges stem from physicians who haven’t seen enough PCOS cases to have symptoms top-of-mind. That’s one of the reasons that specialists are working to create educational materials to empower physicians to diagnose PCOS accurately.
If a woman demonstrates at least two of these three symptoms, a doctor can offer a PCOS diagnosis:
- Irregular menstrual cycles.
- Excessive hair growth (signaling elevated levels of male hormones called androgens).
- Polycystic ovaries (possibly enlarged ovaries showing many follicles).
Yet many women display only one of the three, and doctors must dig deeper using blood tests and additional symptoms to diagnose PCOS.
Infertility issues
After receiving her diagnosis, Allen was relieved that her weight gain and malaise wasn’t all in her head. She turned to the internet to learn what living with PCOS meant.
“The first thing I learned is that the internet can scare the heck out of you,” Allen says.
Myths persist online, including that PCOS is a death knell for a woman’s fertility. But while PCOS is a common cause of infertility — due to hormonal imbalances that interfere with ovulation — it is treatable.
Asima Ahmad, MD, a reproductive endocrinologist with Fertility Centers of Illinois, isn’t just a fertility specialist. She also has PCOS, a nuance that can help her patients feel more at ease with their own diagnosis. And she wants to make sure patients know that despite the internet’s best intentions, PCOS isn’t a “diagnosis of doom.” In fact, one of her favorite parts of working with women with PCOS is dispelling myths and giving them hope.
“Once a patient has a PCOS diagnosis and they know it’s contributing to her fertility challenges, we work together to find things that can help her manage symptoms and increase her chances of achieving pregnancy,” Ahmad says. “There are ways you can conceive. You can still live a long, healthy life after a PCOS diagnosis.”
Once diagnosed, women with PCOS are generally advised to make multiple lifestyle changes to manage symptoms. Healthy eating and weight loss can help control multiple symptoms, from regulating how the body uses blood sugar to making periods more regular.
Multiple medications might be explored to find the ones that work best, including birth control pills to regulate periods, anti-androgen medications to control unwanted hair growth and the drug metformin to decrease insulin resistance and induce ovulation.
Moving forward
Allen worked with fertility expert Angeline Beltsos, MD, at Vios Fertility Institute, to explore ways to preserve her fertility, which included freezing her eggs. “I knew I wanted children someday, even if that wasn’t right now, and I didn’t want a condition to get in the way of that,” Allen says.
In 2018, at age 31, Allen harvested and froze her eggs. She now has 27 viable eggs waiting for her when she’s ready to pursue a pregnancy. And she’s heartened by knowing that her best friend, who also has PCOS, recently gave birth to her first child.
“It gave me hope,” Allen says.
As Allen looks to her future, she has a new appreciation for the resources the internet has to offer: support groups.
“I’ve learned so much just from reading the successes of other women with PCOS,” she says. “Every person I’ve met with PCOS is different, and we’re all just trying to find what works and ways to move forward.”
It’s not the win Allen was expecting, but she’ll take it.