5 common causes of peripheral neuropathy
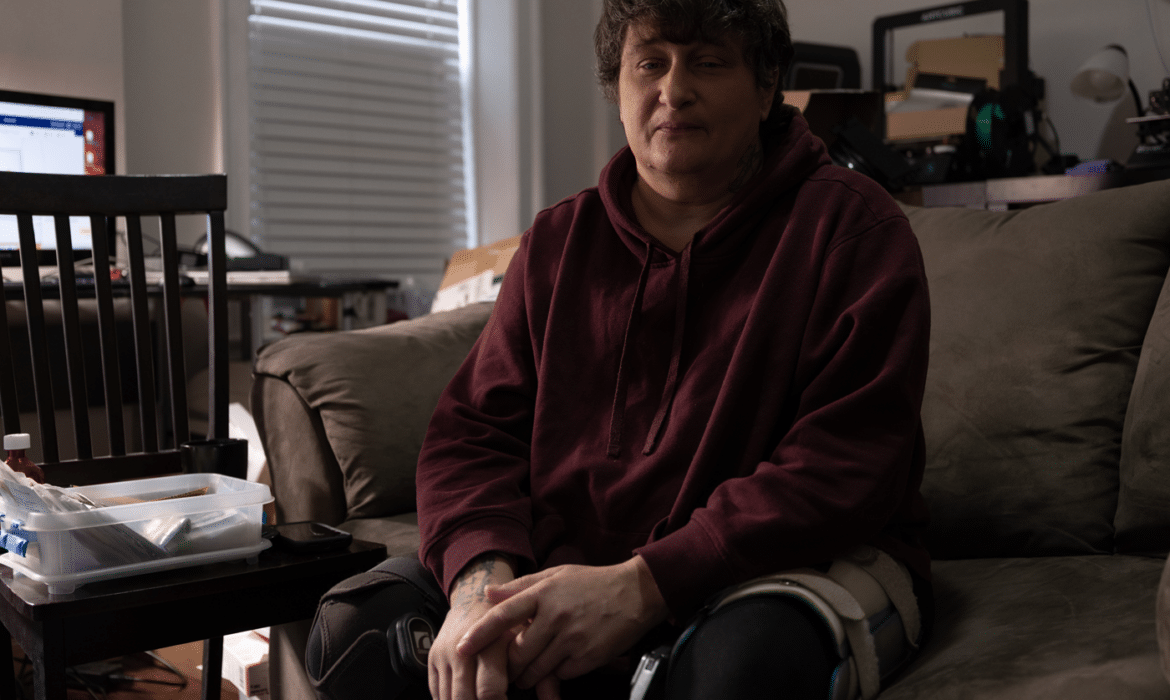
At 7 weeks old, Angel Mason’s doctor diagnosed her with type 1 diabetes. Twenty years later, she developed diabetic neuropathy. It’s the most common form of peripheral neuropathy — a degenerative nerve disease that causes numbness, pain, and disability.
Some 20 million Americans — most over age 50 — have neuropathy. The condition affects nerves’ ability to transmit and interpret signals from the brain and spinal cord.
Peripheral neuropathy begins at the outlying areas of the body, such as the feet. It then gradually spreads to the legs, raising a person’s risk of falls and disability.
Like Mason, most people with diabetic neuropathy know they need to check their feet carefully for sores and infection. Neuropathy might keep them from feeling an injury, and poor blood flow to the area hinders the body from healing injuries or infections.
As the condition progresses, it gets more complicated. “It’s in my feet, legs, and hips — it’s everywhere. It feels like my skin is on fire. It never stops,” Mason says. Now 60, she works as an herbalist and runs a virtual chronic pain support group from her Rogers Park home.
Both Mason and neurologist Rabia Malik, MD, of Rush University Medical Center, say everyone, especially people with diabetes, should take neuropathy seriously.
“Even prediabetes can cause neuropathy,” Malik says. Catching it early opens up more treatment options, more potential to slow the disease’s progression.
“When you can’t feel changes in your body, and you have numbness, it’s so important to get the proper medical care.”
Early-stage peripheral neuropathy treatments include medications such as gabapentin, pregabalin, and duloxetine. Topical gels and creams made with capsaicin (cayenne pepper) may help, too. And many people also turn to medical marijuana, with varied results, Mason says.
“Poor nerve health is often accompanied by chronic inflammation and oxidative stress, which exacerbate challenges to attaining optimal nerve health. Many of the supplements that support nerve health have antioxidant properties,” says Lindsay Colbert, executive director of The Foundation for Peripheral Neuropathy.
Diabetes isn’t the only cause of peripheral neuropathy. Here are four other reasons people may develop this painful and progressive nerve issue:
Severe alcohol use.
People who drink to excess over many years may eventually lose feeling in their feet and legs, to the point that they can’t walk on their own. Alcohol, a toxic central-nervous system depressant, damages nerves over time, just as high blood sugar does in people with diabetes. Excessive alcohol consumption can also crowd out other helpful nutrients, leading to anemia and nutrient imbalances.
Vitamin B12 deficiency.
Plant-based diets are healthy, but if you’re on one, check your vitamin B12 levels. This key vitamin enters the body through animal protein. A lack of B12 can lead to peripheral neuropathy if not treated carefully with either dietary changes or B12 injections. Without B12, the body produces too-large red blood cells that don’t carry enough oxygen. The lack of oxygen damages the myelin sheath surrounding our nerves.
Low thyroid levels.
Also known as hypothyroidism, low thyroid can lead to peripheral neuropathy and nerve damage. Researchers don’t fully understand the link
between hypothyroidism and peripheral neuropathy, but the condition can cause fluid retention, which puts pressure on peripheral nerves. Malik says anyone with symptoms, such as numbness or tingling in hands and feet, should have their thyroid levels and other key neuropathy markers checked.
Cryptogenic sensory polyneuropathy.
This slowly progressive disease in older adults typically causes pain and numbness without significant muscle weakness, Malik says. The condition appears to affect the axons (or core of the nerve) with early involvement of the long nerve endings, according to National Institute of Health researchers. Luckily, most people who have it are still able to walk independently.
Other, lesser known causes of neuropathy include autoimmune diseases that damage the nerves, infectious diseases, and viral infections, including Guillain-Barré syndrome. syndrome. Researchers are also looking into nerve and muscle damage from Covid-19.
For Mason, following a vegan, anti-inflammatory diet has given her the most control over her pain. She avoids fast food, sugar, corn syrup, alcohol, and trans fats. Research has yet to zero in on promising treatment options, she says, but she has hope for new gene therapies on the horizon.
“There is a lot of interest in the medical community in better diagnosing, managing, and understanding the mechanism of nerve injury. For example, spinal cord stimulators can be used in certain cases to help with pain management,” Malik says. “Current research in neuropathy also focuses on nerve regeneration rather than alleviating symptoms alone.”
Meanwhile, alternative medicine options provide some relief. “Nutrition, supplements, and acupuncture can help,” Malik says.
Whether people use traditional or integrative medicine, it’s important to find credible and trustworthy providers, says Ronald Lissak, board member of The Foundation for Peripheral Neuropathy, based in Buffalo Grove. “When you can’t feel changes in your body, and you have numbness, it’s so important to get the proper medical care,” he says. “Don’t let things fester.”
Colbert cautions people experiencing neuropathy to be savvy health consumers and avoid advertisements promising a cure. “The bottom line is that if someone is promising a cure, it’s not real,” she says.
When in doubt, Colbert recommends people check with their primary care doctor or contact the foundation to verify a treatment at: foundationforpn.org.
Family, peer, and mental health support are key. People experiencing neuropathy often experience depression and isolation as the result of constant pain. “One of the issues with chronic pain is that it’s invisible. We try to put on a smile and say, ‘I’m ok,’” Mason says. “Most people don’t understand. That’s why I started this group.”
Mason’s Chicago Chronic Pain Support Group meets from 6 to 8 p.m., the second and fourth Wednesday of the month. For the Zoom link and details, contact Mason through her website at ihurtchronicpain.com.
Above photo: Angel Mason. Photo by Jim Vondruska
Originally published in the Spring/Summer 2023 print issue.