From telehealth to magnetic stimulation, innovative therapies provide alternatives
At the end of the 19th century, it wasn’t uncommon for those suffering from depression to spend a stint in a sanitarium. Never mind that it would have been framed that they’d “gone to visit relatives.” A century later, more than 16 million people in the United States live with a diagnosed major depressive disorder. That’s a lot of trips to “visit relatives.”
The good news is this: The treatments for depression are more plentiful and diverse than ever. No matter the severity of a patient’s experience with depression, there are choices that go well beyond an inpatient stay or an orange bottle with a childproof cap. Here are some of the approaches leading the way in depression treatments today.
The rise of telemental health
Technology makes it possible for mental health professionals to reach patients well beyond their office walls. If you live in a remote area or prefer the privacy of your own home to a mental health professional’s office, telemedicine can help you access the help you need, when and where you need it.
“Originally, telemental health was focused on providing psychiatric treatment to those living in hard-to-access areas,” says Peter Yellowlees, MD, MBBS, professor of psychiatry at UC Davis and past president of the American Telemental Health Association. “Today, it’s more about convenience and being able to connect in a hybrid fashion, allowing patients to conveniently see providers in person and online.”
Through secure web-based messaging and video-conferencing applications, those suffering from depression can now close a door or discretely send a message to their mental health professional for regular, private care at home. They usually will still visit their psychiatrist on a limited basis and have their treatment plan managed by their primary care physician.
“We used to use technology to provide better access in hopes of providing as good care as we would for patients in our offices,” Yellowlees says. “Now, we’re providing better access that gives patients better care.” That means rural patients receive more regular therapy appointments and medication reviews, and those seeking discretion receive the treatment they need on a regular basis through a private medium they feel comfortable with.
Personalized medicine
For all the medications available for depression, there’s still the question of which one will work for which person. Many times, people switch from drug to drug, suffering side effects until they find what is most effective for them. That’s a puzzle that Joshua Straus, MD, a psychiatrist at NorthShore University HealthSystem, is working to solve through pharmacogenomics.
“The main idea behind pharmacogenomics is that ways people respond to medications may be inherited,” Straus says. “Genetic testing can tell us if a particular medication might break down too fast or too slow in someone’s body, respectively rendering it ineffective or giving unpleasant or even dangerous side effects.
“It’s not a silver bullet,” he says, “but it can help us treat those suffering from depression in the ways that an MRI or other diagnostic tests can assist in assessing and treating other medical conditions.”
Straus recommends pharmacogenomic testing for those who’ve had poor results with a few depression medications, including adverse side effects, dosage challenges and low to no results. The costs are accessible (under $255 through Straus’ program) and insurers are beginning to cover the testing costs for some patients.
“This testing can increase the odds that they’ll end up on a medication with positive effects,” Straus says. The best way to begin with pharmacogenomics is to start a conversation with your primary care physician or psychiatrist, he adds.
Exploring TMS
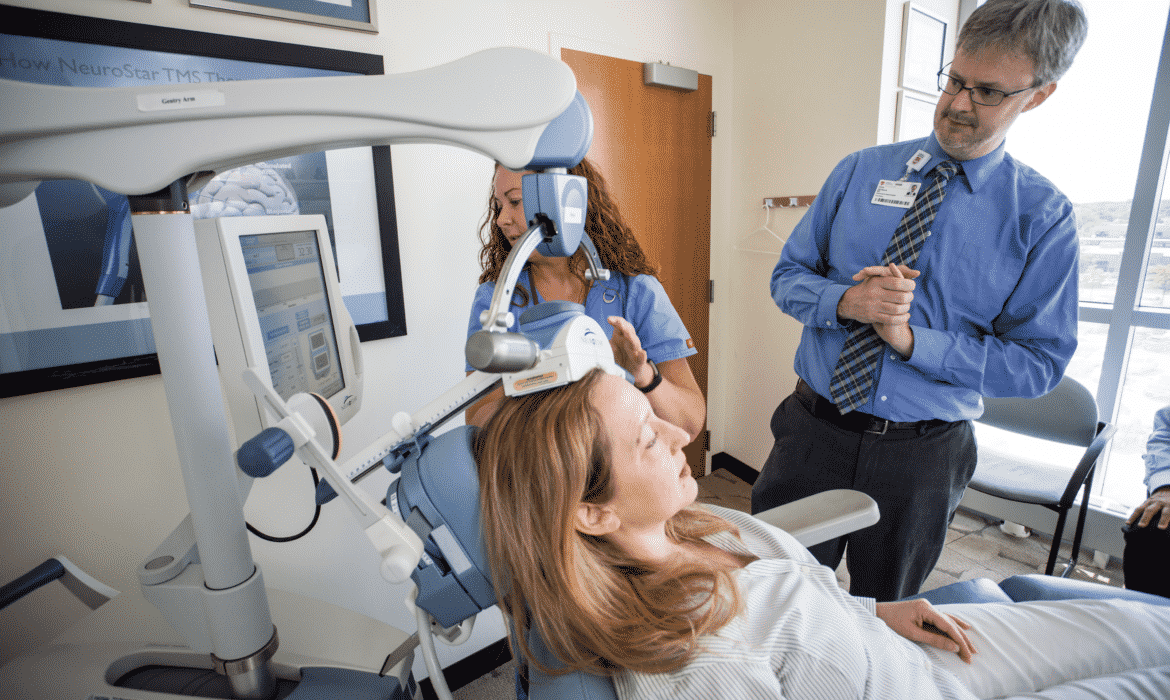
For those who’ve found medications to be frustratingly ineffective, a new type of treatment is offering hope. Repetitive transcranial magnetic stimulation (TMS)
is an FDA-approved, non-invasive and non-medication-based treatment for major depressive disorder for those who have failed to respond to at least one medication trial.
This testing can increase the odds that they’ll end up on a medication with positive effects.”
In a TMS session, which lasts about 20 to 40 minutes, a small electromagnetic coil positioned on the surface of the head delivers a series of brief magnetic pulses to the cortex of the brain. When done five days per week over a four- to six-week period, patients can sometimes experience significant improvements in depressive symptoms, says Evan Deranja, MD, PhD, associate professor and associate residency program director at the Psychiatry and Behavioral Neurosciences Department at Loyola Medicine.
“For most people the stimulus feels like a light woodpecker tapping on their head whenever the magnet is delivering pulses,” Deranja says. “The beauty of this treatment is that not only does it work, but also it is non-invasive and does not require the patient to be continuously using it on a long-term basis, as does a medication.”
TMS offers an alternative for those who have found medication protocols unsuccessful. While it’s not 100 percent effective for all patients with depression, Deranja reports that approximately one-third of all patients have a “very good response” and achieve remission of their major depressive episode.
A 2014 study published in the Journal of Clinical Psychiatry showed that 30 percent of those with treatment-resistant depression achieved remission with TMS treatment. Another study showed that 70.5 percent of patients who achieved full remission did not relapse over the next year.
Intensive depression treatment programs
But what if you need more intense care and find your quality of life impacted by your depression?
The word “intensive” might sound daunting, yet patients at Rogers Behavioral Health in Skokie would beg to differ. Rogers has created programs that can help those living with depression approach their treatment on a more intensive and accelerated track than typical once-a-week therapy sessions can facilitate.
“Our programs provide patients a higher level of support,” says Paula Young, PhD, clinical director of Rogers Behavioral Health–Chicago. Intensive outpatient and partial hospitalization programs are geared toward those who have impairments because of mood and anxiety disorders, as well as those who are struggling to do their work because of their depression.
Rogers offer patients both partial hospitalization and intensive outpatient treatment options, with patients receiving significant one-on-one time with mental health care professionals in addition to group-based work to teach skills essential for coping with depression in their daily lives.
The intensive programs can be powerful solutions for those who find that depression interferes with participation in daily life, like those who have dropped out of school or are on disability or medical leave from work.
“While once-a-week therapy options leave a lot of days in between without support or accountability, our programs help patients access a higher dose of therapy and behavioral treatment on a daily basis, which can speed a patient’s return to work, school and life in general,” Young says.
From telehealth to more targeted courses of treatment, it’s clear that those living with depression have more options than ever before. For those who suffer, support and guidance from qualified, licensed mental health professionals is never far away. However depression impacts a person’s life, there are treatment options that offer both privacy and support and prevent patients from having to “visit the relatives.” Because we all know how stressful that can be.