It’s winter in Chicago, and due to the Covid-19 pandemic, we’re indoors more than ever. This spells trouble for skin.
Outside it’s cold and crisp, while inside radiators and furnaces blow dry heat. We seek hot baths and showers, which further dry out our skin. And then there’s the ever-present worry of the pandemic, which also stresses our system.
Itchy winter skin is especially hard for people with the chronic condition eczema, also called atopic dermatitis.
“We’re living in a time of super-high emotional stress, which can increase the inflammation in our skin,” says Amanda Wendel, MD, a dermatologist at Northwestern Medicine Central DuPage Hospital. “Our skin is suffering more now than ever before.”
Eczema is known as the “itch that rashes,” because the itch starts first and then an angry, persistent rash follows.
Once the uncomfortable itching begins, rough or thickened plaques, scaly lesions, or raised hives can form and spread, says allergist Rachna Shah, MD, of Allergy, Sinus, & Asthma Professionals in Oak Park. Common flare-up spots include elbows, hands, ankles, and behind the knees. But the rash can show up anywhere, Shah says.
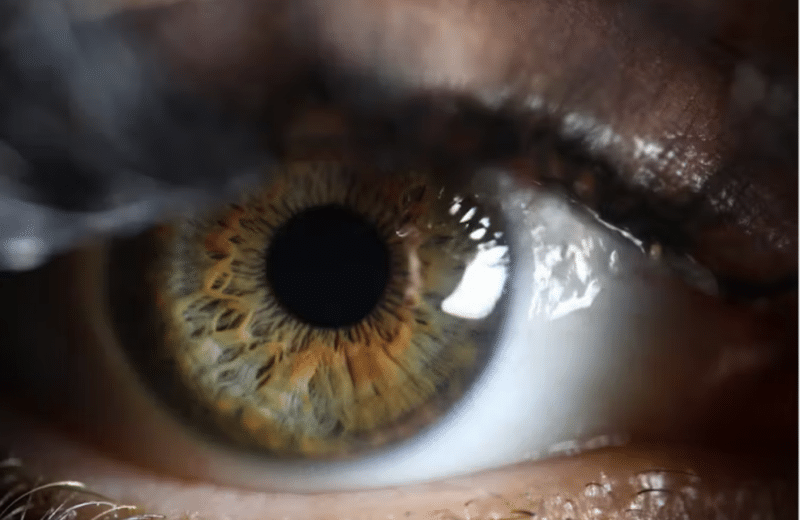
In eczema, the body’s immune system sends out signals that cause inflammation, itch, and damage to the skin barrier. Itch nerves, similar to pain nerves, signal up through the spinal cord to the brain, explains Peter Lio, MD, dermatologist at Northwestern Medicine. When we scratch the itch, the action of the fingers transmits a low-level pain signal that overrides the itching sensation and causes a momentary distraction, which increases the feeling of relief.
The skin is a barrier that prevents pathogens from entering the body and also prevents the skin from losing moisture.
“We have learned that in patients with eczema, the skin barrier is not functioning properly, resulting in a state I call leaky skin,” Lio says. “When the skin barrier is malfunctioning, water can escape too easily, resulting in dry, flaky skin that often can’t seem to hold on to moisture. Allergens, irritants, and pathogens can abnormally enter the skin, causing the immune system to get even more activated, further driving allergy and inflammation.”
Irritants and allergens include dry atmosphere, changes in temperature, stress, cleaning products, soap, hair dye, synthetic clothing, wool clothing, dust mites — the list goes on and on.
As if that wasn’t enough to contend with, 25% to 50% of people with eczema have a mutation of the gene encoding filaggrin, a structural protein of the skin that provides a natural moisturizer, according to the journal Allergology International. This enables allergens to penetrate the skin, leading to a weakened epidermal layer.
“The hard part about eczema is that it is multifactorial. It’s generally not as simple as one thing being awry,” says Lio, who recommends downloading the free app EczemaWise to track skin condition and identify triggers, insights, and trends.
With all of these complex aspects, figuring out the root cause of eczema can be quite puzzling. Consider these five steps to find your skin solution:
1. Sustain skin hygiene
Because their skin barrier often is compromised, people with eczema are more susceptible to secondary infections caused by skin bacteria and pathogens. This makes skin hygiene key, including keeping skin clean and moisturized.
“Take a five- to 10-minute lukewarm shower or bath daily,” Shah says. “This will keep the skin clean and add back some moisture.”
It’s tough not to turn the water to hot, but it’s important to opt for a lukewarm temperature, Shah says. Run the water over your wrist. If it feels warmer than your body temperature but not hot, that’s where you want it to be.
When it comes to cleansers, use unscented, gentle options. Shah recommends products like CeraVe — which contains ceramides, a type of lipid that helps retain moisture in the skin barrier — and Cetaphil.
“After the shower, pat dry,” Shah says. “Even though rubbing your skin with the towel would attain instant itch relief, this will only lead to more microtears,” Shah says.
Afterward, moisturize with a quality moisturizer. Unscented, thick creams work better than lotions. Also, look into sensitive skin lines with minimal ingredients and anti-inflammatory compounds.
2. Check your home humidity
In Chicago’s dry, cold winter, it can be difficult to maintain your home’s indoor humidity.
“For skin health, the humidity in your house should be 30% to 35%,” says Shah, who recommends placing a humidifier in the room where you sleep or work. “You can opt to just leave it on for two hours to avoid too much moisture, which can trigger other allergies,” she says.
Clean humidifiers weekly with white vinegar, bleach, and a small brush, because microbes can grow in the reservoirs and make their way into the air.
To test humidity levels in your home the old-fashioned way, fill a glass with water and place two or three ice cubes in it. Then, wait about four minutes. If excess condensation forms on the outside of the glass, your humidity levels may be too high. On the other hand, if there is no condensation, your humidity levels may be too low.
3. Be cautious about clothing
If you’re looking for relief from eczema’s itch, think about anything that touches your skin, including your clothing and your laundry detergent, which should be free from fragrance, one of the most frequently cited substances causing flare-ups, according to the National Eczema Association.
For a long time, cotton and silk were the go-to fabrics for people with eczema, but a 2020 study published in the American Journal of Clinical Dermatology says that synthetic antimicrobial and moisture-wicking fabrics may help reduce eczema symptoms.
A study published in Clinical, Cosmetic and Investigational Dermatology found that sleep improved for eczema sufferers who wore long sleeves and long pants made of antibacterial zinc fibers for three nights in a row.
4. Treat persistent symptoms
Treating eczema is not always straightforward, because there’s more involved than just a rash. Thankfully, there are ways to soothe the immune response and minimize inflammation.
Taking a daily 24-hour antihistamine, such as Claritin, Zyrtec, or Xyzal, can help control the itch, Shah says. “This will help keep allergic-related symptoms under control, which could mean less itching for you.”
Topical creams can help soothe the immune response. Often doctors prescribe corticosteroids, but some nonsteroidal treatments may help too. “While topical steroids can be very helpful, we have to be mindful of not overusing them because they can thin the skin barrier and users can become overly reliant on them,” Lio says. “Nonsteroidal treatments can help minimize steroid use to keep the skin safe.” Such treatments include crisaborole, sold under the brand name Eucrisa.
Beyond this, dermatologists may move to things like wet wrap therapy, which involves wrapping affected areas with damp fabric. Also, phototherapy uses UV light treatments that have an anti-inflammatory and antibacterial effect on the skin. The treatment can “safely and effectively” treat eczema, according to the American Academy of Dermatology Association.
For people with moderate to severe eczema who haven’t gotten relief after using topical or alternative treatments, there’s the newest biological drug dupilumab (Dupixent). This drug — self-administered biweekly by injection — contains an antibody that inhibits inflammation.
5. Explore possible food triggers
Many patients and families are convinced that food is the root cause of eczema, or at least an important trigger, Lio says. “But for most of our patients with eczema, food seems to play a relatively small role in actually driving the skin disease.”
“The whole thing is very complex because, undoubtedly, food allergies are associated with atopic dermatitis, and around one-third of moderate or severe atopic dermatitis patients have actual food allergies,” Lio says. The most common are allergies to cow’s milk, eggs, nuts, fish, soy, and wheat.
An allergist can use a skin prick test or blood test to diagnose an allergy. But even if you’re not allergic to a food, it still may affect eczema.
“Unfortunately, there is more to the story,” Lio says. “Some foods seem to be inflammatory in a nonallergic, less specific way, such as dairy products. For some people, consuming a lot of dairy seems to make things worse,” in terms of atopic dermatitis or acne. “This is not a true allergy, but it does seem to drive inflammation.”
While there are tests for food allergies, there are no established tests for food sensitivities. The best way to determine if you’re sensitive to a food is to try an elimination diet, eliminating a specific food category for two weeks to see if your symptoms resolve and then gradually reintroducing it to see if symptoms recur.
“For adults, I do think it is fine to experiment with avoiding a certain food for a bit if there is something that they are convinced is making things worse,” Lio says. “I also like to guide patients more generally on a healthy diet: plant-based, cutting out processed foods as best they can, eliminating sugary foods, focusing on home-cooked fresh and whole foods.”
Although it’s tricky to stop eczema, starting with the five steps above could help the persistent itch finally fade.