Chicago programs help young victims of trauma find their way forward
“What happened to you?”
Asking troubled children that question instead of, “What’s wrong with you?” is the basic premise of trauma-informed care.
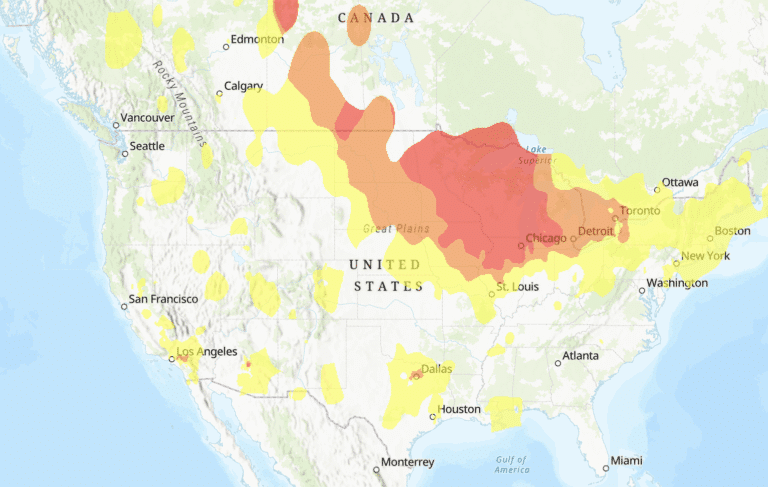
Childhood trauma occurs when a youth experiences an event that is emotionally painful or distressful, such as gun violence, sexual abuse, domestic violence or witnessing a death. Trauma can also result from an ongoing stress, like community violence or poverty — issues that unfortunately are prevalent in Chicago. These powerful events can overwhelm a child’s capacity to regulate emotions, and they often have lasting mental and physical effects.
“Problem child,” “juvenile delinquent” and “bad seed” are broad terms that used to be applied to violent or disruptive children, and their behavior was traditionally treated with punishment or shame. However, we are starting to learn more about why children exposed to trauma seem more likely to lash out, run away or use drugs.
Trauma’s lasting effects
Research, like the landmark 1998 Adverse Childhood Experiences (ACE) study, has established that the more a child is exposed to adverse experiences, the greater likelihood of behavioral problems, substance abuse, poor mental health and chronic diseases like heart disease, liver disease and autoimmune disorders later in life. Additionally, many specific forms of trauma occur in conjunction with others. For example, the ACE study showed that among adults who reported sexual abuse, 65 percent reported at least one additional adverse childhood experience and 41 percent reported at least two.
Brain imaging studies show that those who’ve had adverse childhood experiences have changes in the structure and function of areas of the brain responsible for memory, learning and emotions. An early traumatic event can affect a child’s ability to cope with future stressor setbacks, leading to a greater likelihood of negative coping mechanisms like substance abuse, disordered eating and violence.
Trauma-informed care provides support services and appropriate coping strategies so individuals are better equipped to handle future challenges. With this approach, therapists, educators, social workers and foster care agencies can help children learn to respond to stressful situations without resorting to violence, withdrawal or self-harm.
“What are the developmental gaps that occur as a result of trauma in the absence of sufficient protective factors?” asks Audrey Stillerman, MD, a family doctor at UI Health who is studying with the Houston-based ChildTrauma Academy. “If we can identify them, what can we do to support that development so that we can heal the brain and help people realize their optimal potential?”
From schools to healthcare settings, more specialists are changing their approach to care, recognizing that trauma experienced in childhood can cause a cascade of physical and mental health effects later in life. And this acknowledgment is where healing begins.
Get curious, not furious
After her difficult divorce, Denise Lopez’s teenage son was demonstrating concerning behavioral issues. “He’d get upset right away and lash out” when they’d argue, she says. “He’d punch the wall and try to burst out of the house.” His school principal suggested that she send him to a behavioral hospital. Lopez decided to send her son to the therapeutic residence program at Mercy Home for Boys & Girls.
Mercy Home’s clinical director Emily Neal, LCSW, says that the majority of children at Mercy Home for Boys & Girls are survivors of some sort of trauma or adversity. Clinicians at the program are trained in a trauma-informed model called Attachment, Regulation and Competency (ARC). The ARC model, Neal says, provides an alternative to more punitive responses to behavioral problems like violence. Therapists address the reasons behind the behavior while teaching residents emotional management techniques.
At Mercy Home, Lopez and her son learned techniques to control his emotions. “If he’s yelling, I’ll say, ‘Let’s have a seat. Let’s breathe. Let’s talk about how you’re feeling,’” Lopez says. “He’ll tone it down. Before, he wouldn’t.” She also came away with her own management strategies. “They’ve shown me you need time for yourself. Take a walk around the block, read a book, journal. If I’m not mentally stable, my kids won’t be.”
Wounded warriors
The effects of trauma can be both intergenerational and contagious. When veterans suffer from post-traumatic stress disorder (PTSD), their loved ones may suffer, too.
At the Road Home Program at Rush University Medical Center, providers offer counseling to veterans as well as their families. “We talk about managing trauma reminders so [a parent’s PTSD] isn’t such a mystery” for children, says Jonathan Goldner, PhD, a psychologist at the program.
“A family may be asked, ‘What are the things that are hard for Mom or Dad?’ and told to list which situations might generate flashback reactions that could frighten a child,” he says.
Goldner wants to see widespread use of trauma-informed care in schools, especially those serving at-risk youth. “The alternative is that we view them as problem kids, and we don’t understand them for who they are and what they’ve been through.”
Creating healing school communities
Trauma-based care is provided to children at the Center for Childhood Resilience, the community outreach arm of the department of child and adolescent psychiatry at the Ann & Robert H. Lurie Children’s Hospital of Chicago. However, a major part of the center’s work is making sure that treatment is available to children where they spend most of their time — in school.
“We know that nationwide about 20 to 25 percent of kids who need mental health care receive it, and 70 to 80 percent of those who get mental health services get them in the school setting,” says Tali Raviv, PhD, pediatric psychologist at Lurie Children’s Hospital.
At the center, community-based mental health providers train educators, librarians and after-school program administrators in two evidence-based interventions: Bounce Back, for elementary school students, and Cognitive Behavioral Intervention for Trauma in Schools (CBITS), for grades 5 to 12. Clinicians also train teachers to spot signals that students may need more intensive trauma-informed care.
Counselors at Newton Bateman Elementary School in Albany Park went through Bounce Back training in fall 2017 and began using it immediately. “We had a number of children we kept in mind at Bounce Back training,” says Bateman social worker Elizabeth Asher. “We were [thinking], ‘Yes, we know exactly who needs to go to this group.’”
Some children at Bateman have gone through harrowing experiences, like fleeing domestic violence or being involuntarily separated from their parents. “These children become easily emotionally triggered by the traumas they experienced, which affects their social and academic functioning,” Asher says.
Bounce Back training taught the counselors how to better take children’s trauma histories, as well as how to employ relaxation and breathing exercises that can help them cope in difficult moments. The Bateman teachers already have reported fewer incidents. “I think [Bounce Back] should be in every school,” Asher says.
Through the fire
When a patient is flagged for having survived a violent incident like a shooting, Healing Hurt People–Chicago steps in at the John H. Stroger Jr. Hospital of Cook County and UChicago Medicine Comer Children’s Hospital.
“Our goal is to have contact with them as early as possible and to provide some basic education about trauma and ways to manage that,” says UChicago psychologist Bradley Stolbach, PhD, the program’s clinical director.
As a hospital-based violence intervention program, Healing Hurt People replaces the protocol of merely treating someone’s physical injuries and sending them home.
Healing Hurt People connects patients with various resources to help. One such resource is Project FIRE (Fearless Initiative for Recovery and Empowerment), created by Stolbach and glass artist Pearl Dick. The program provides at-risk Chicago youth a confidence-building blend of arts education, mentoring, trauma education and employment. Typical sessions at the Firehouse Art Studio consist of three hours in the “hot shop” to create colorful, captivating glass sculptures, followed by one hour of snacks and a trauma psychoeducation group.
These children become easily emotionally triggered by the traumas they experienced.”
Glassblowing, Stolbach says, is a therapeutic medium for victims of violence. “You have to pay attention to how you’re moving, what the glass is doing, who else is around you,” he says, which helps participants be themselves and feel present. The employment aspect of selling glasswork is especially meaningful, Stolbach says. “It’s only a few hours a week, but for a lot of our kids, having a job is really a big deal. They can say, ‘Oh, I have to go to work,’ and they’re getting a paycheck.”
Creative therapy methods like the glassblowing program recognize that some children benefit from sensory and body-based interventions designed to help repair the brain with repetitive motion-based activities.
“Art therapy provides somatosensory experiences,” Stillerman says. “If we can restore the rhythmic stimuli we experienced in the womb, it really helps us access higher parts of the brain.”
Of healthcare and hope
There is hope for childhood victims of trauma. In 2017, Senator Dick Durbin introduced the Trauma-Informed Care for Children and Families Act, which would make it easier for more families to gain access to trauma-based therapy. However, the bill is still in committee and has yet to be presented to the Senate.
Action is also taking place within
the therapeutic community. Stillerman co-founded the Center for the Collaborative Study of Trauma, Health Equity and Neurobiology (THEN) with the goal to create an institute in Chicago that will develop trauma training programs and resources.
An entire generation could be helped with the right care, whether it’s trauma-specific therapy or simply a listening ear, Raviv says.
“Many people who have had exposure to trauma go on to live really productive lives,” she says. “[Children] are resilient if they have a good support network and if they have links to programs that can [help] them thrive.”
Traumatic experiences in childhood can lead to major problems later on, including:
- Alcoholism and alcohol abuse
- Chronic obstructive pulmonary disease
- Depression
- Fetal death
- Illicit drug use
- Ischemic heart disease
- Liver disease
- Poor work performance
- Financial stress
- Risk for intimate partner violence
- Multiple sexual partners
- Sexually transmitted diseases
- Smoking
- Suicide attempts
- Unintended pregnancies
- Early initiation of smoking
- Early initiation of sexual activity
- Adolescent pregnancy
- Risk for sexual violence
- Poor academic achievement
Source: Centers for Disease Control and Prevention (CDC)