New initiatives encourage transplantation instead of costly dialysis
Nancy Nora, MD, had long considered donating one of her kidneys. As a nephrologist with NorthShore University HealthSystem in Highland Park, she specializes in kidney disease and knows better than most about the need for organ donors.
About 15% of U.S. adults have chronic kidney disease, often brought on by diabetes or high blood pressure. As chronic kidney disease advances, it can result in end-stage renal disease, with patients needing either dialysis or a kidney transplant to survive.
That complex and costly progression takes a toll on people’s quality of life.
A new federal push aims to increase kidney transplants in order to combat the rising incidence of kidney failure and the high cost of dialysis.
The toll of dialysis
Chronic kidney disease is far more common in people 65 and over. As the U.S. population continues to age, the number of people with the condition — and the corresponding cost of coverage — will continue to rise.
About 80% of those on the kidney transplant waitlist are on dialysis, a treatment that removes waste, salt and extra water from an individual’s blood, because the kidneys are no longer able to do so. But dialysis can be expensive and time intensive.
In hemodialysis, the most common type of dialysis, blood is removed from an individual, filtered through an external device and pumped back into the body. This process is usually done three times per week, with each session lasting three to five hours.
In peritoneal dialysis, cleansing fluid runs through a catheter, which is inserted into an individual’s belly to filter waste. Individuals can complete the treatments at home, though they need to do it several times each day.
You can survive and do quite well with one kidney, and what a wonderful gift it is to give to someone.
The treatments can be extraordinarily expensive. Medicare covers approximately $28 billion in costs for hemodialysis care annually, while spending for transplant care is about $3.4 billion.
Not only do kidney transplants cost less than prolonged dialysis, but also they’re associated with better quality of life, lower risk of death and fewer dietary restrictions. However, there are some risks from the transplantation surgery and anti-rejection drugs, according to the National Institute of Diabetes and Digestive and Kidney Diseases.
Transplant focus
To address the increased incidence and impact of kidney disease, the federal Advancing American Kidney Health initiative, which kicked off in July 2019, expands reimbursements for living organ donors to increase the number of kidneys available for transplant. The initiative also encourages the development of artificial kidneys.
The transplant process is relatively simple. Most recipients tend to be released from the hospital within three to seven days, while donors are discharged after one to three days — as Nora experienced when she became a kidney donor herself.
With such high demand for kidneys, Nora felt a need to act. She was confident that she’d be able to live a long and healthy life with just one kidney. Her original plan was to save her kidneys in case one of her children ever needed one, but when she found out she wasn’t a good match for her children, she decided to go a different route.
In 2010, Nora donated a kidney to one of her patients who was on dialysis. Nora went into the hospital for surgery on a Thursday, was back home the next day and returned to work the following Monday.
For years, Nora didn’t publicize the transplant, but when she realized it could encourage others to follow in her footsteps, she was happy to share her story.
“The techniques and the medication needed to preserve transplants have gotten much better,” Nora says. “We both haveexcellent kidney function. You can survive and do quite well withone kidney, and what a wonderful gift it is to give to someone.”
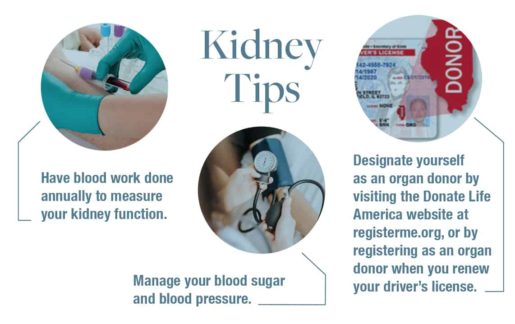
Increasing knowledge
Nine out of 10 people with chronic kidney disease don’t know they have it, because people rarely experience early symptoms, according to the Centers for Disease Control and Prevention. By the time nausea and fatigue come into play, the disease is usually well advanced. The best way to catch kidney disease early is to see a physician annually or at least have blood and urine tested once a year to measure how quickly body waste is being removed.
“Part of this [Advancing American Kidney Health] initiative is to identify the kidney disease as early as possible and take steps to intervene and improve care so patients can potentially stave off initiating dialysis,” says Yolanda Becker, MD, director of the kidney and pancreas program at UChicago Medicine.
The National Kidney Foundation’s “The Big Ask, The Big Give” campaign addresses individuals who are considering donating a kidney while they are living or after they have passed away, as well as those who are in need of a kidney but unsure how to ask for help.
The program strives to disprove common misconceptions about kidney transplants. For example, kidney donors can live a long and healthy life with just one kidney, as Nora has shown. And, contrary to some myths, being marked as an organ donor will not impact the medical care given in case of severe injury or illness.
Donors are carefully screened to make sure there is a good fit. A national computer system matches organs to recipients, looking at blood type, wait time, geographic location and medical information.
“When you get evaluated to be a donor, the emphasis is on making sure you are a good candidate, not just to grab the kidney at all cost,” Nora says.
After their successful transplant experience, both Nora and her former patient are in good health with excellent kidney function. And, Nora says, she hopes others will follow her lead.
Above image: Nephrologist Nancy Nora, MD, donated one of her kidneys to a patient. Photo by Jim Vondruska. Originally published in the Spring/Summer 2020 issue.

Marc Zarefsky is a communications consultant who takes complex topics and humanizes them to create engaging content that inspires action.