Whether stemming from a disease or an injury, many of us have orthopedic conditions that affect our joints, bones, and ligaments. Fortunately, recent advances in orthopedic care are making a difference for many Chicagoans.
Orthopedic surgeons are innovators, constantly adopting new technologies — whether robotic-assisted surgery or 3D motion-analysis technology — to refine their approach, giving their patients the best function with optimal recovery.
Knee and hip replacements reduce pain and grant mobility to people with severe arthritis. And advancements in shoulder and elbow replacements increase function, so people can return to the activities they enjoy.
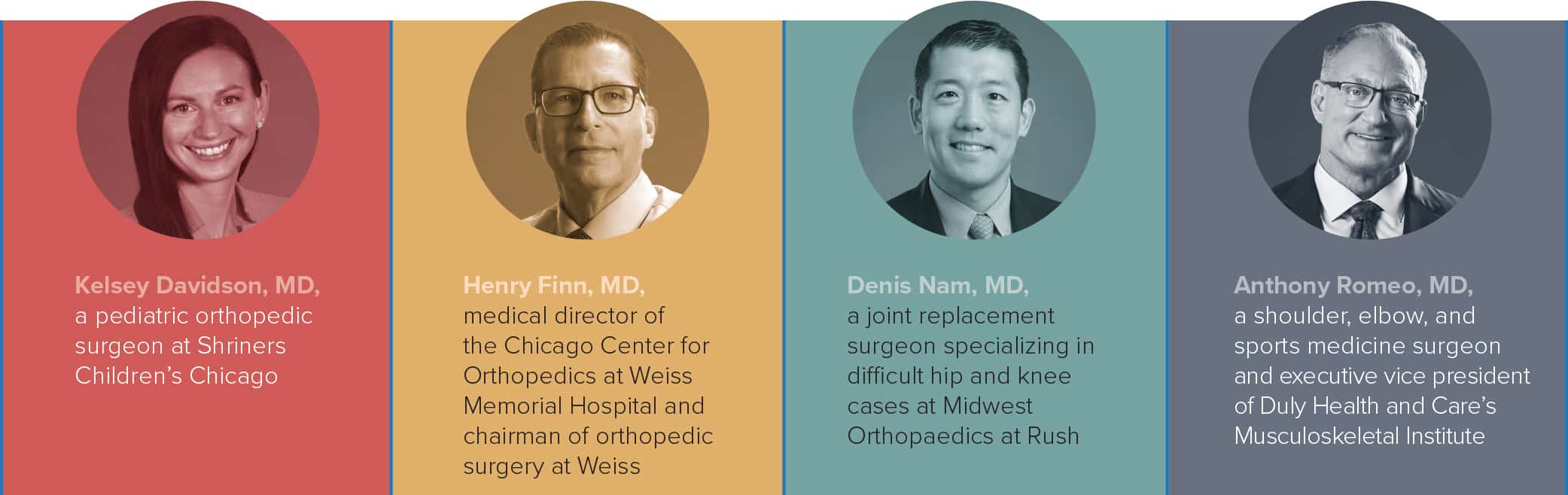
We asked four local leading orthopedists to talk about what these advancements mean. Read on for answers from:
Q: What new developments are you excited about in the field of orthopedics?

Most major implant companies are now introducing robotic systems that provide advantages in the accuracy and precision of placing components during joint-replacement surgery.


I am thrilled to see the development and acceptance of stemless shoulder replacements — which means less bone is removed to secure the implant — for people with osteoarthritis, as well as unique designs of reverse total shoulder implants for people with arthritis and rotator cuff problems. It’s amazing that we can now successfully treat the problems related to cartilage, bone, and tendons with reverse total shoulder replacement.
Also, patient-centered apps and accessible websites allow me to provide individuals with education and expectations before surgery, a better understanding of the surgical procedure, clearly defined rehabilitation exercises, and an effective way to stay in touch after surgery.

At Shriners Children’s Chicago, our motion analysis center provides return-to-sport testing to identify subtle areas of weakness that may increase the risk of reinjury. The information that we provide to the patient can guide rehab and help them safely return to sports.
Q: What questions should I ask my doctor prior to joint repair surgery?

Finally, it is not unreasonable for the patient to ask the surgeon about his or her complication rates. For example, consider asking about the percent risk of infection after surgery.

People should ask surgeons about their specific surgical technique, anesthesia preference, medications, expected road to recovery, and any limitations that they might have after undergoing the surgical procedure. Every physician who performs knee or hip replacement surgery should provide an education class to address patients’ concerns.

• Are you able to do this as a same-day or outpatient surgery?
• Can this procedure be performed in an ambulatory surgicenter instead of a hospital?
• What are the possible complications of this surgery?
• What is the average recovery time with this type of surgery for your patients?
• How long do joint replacements last with your patients?
• Do I have any health conditions that might complicate my surgery or recovery?
• What restrictions will you suggest after I have the joint replaced?
• What help will I need to care for myself after surgery?
• What are my treatment options if I choose not to have surgery?
• How will my condition change or deteriorate if I do not have surgery?
• How many joint-replacement surgeries have you done?

for surgery to minimize stress afterward. Ask your surgeon and care team if you will need equipment to assist with mobility, using the bathroom, or sleeping. Find out if there are devices that can help with surgical pain. In addition, ask how to optimize your health before surgery to aid your recovery afterward.
Having surgery can be very stressful, both physically and mentally. Make certain you understand the goal of the surgery and feel comfortable with the plan. If not, ask your care team about other options or getting a second opinion. This way you can feel confident and prepared for surgery.
Q: Considering the risks that opioids pose, what’s the best way for people to manage pain before and after surgery?

For the surgical procedure and immediately after surgery, my patients follow Enhanced Recovery After Surgery (ERAS) protocols to minimize the effects of anesthesia, reduce post-op pain, and speed recovery. These protocols include best practices from just before surgery to afterward.
Another important aspect includes good nutrition before surgery, so the body has what it needs to heal. Working with our anesthesiology team, my patients drink an electrolyte drink four hours before surgery since this has been shown to help with post-op recovery.
Also, for most upper extremity surgery including shoulder replacement surgery, I use nerve blocks whenever possible, so individuals have up to 12 hours of a painless shoulder after they are discharged home on the day of surgery. This enables them to return to the comfort of their home and settle in the same day as their procedure.

Following surgery, a multimodality approach to pain control includes neuraxial anesthesia (spinals and blocks), anti-inflammatories, intravenous Tylenol, inhibitors of neurologic pain such as Lyrica, systemic steroids, and local infiltration of the tissues with medications that fight pain, swelling, and inflammation. The judicious use of opioids may be considered, being mindful of their complications and risks.

Other modalities include the use of ice, elevation, injections, physical therapy, and also anti-inflammatories. Your physician should provide you with recommendations on what approaches may be most appropriate based on your condition.
Following surgery, one of the greatest advancements has been the use of multimodal analgesia protocols that may include regional anesthetic blocks and a combination of medications that act together to reduce pain through different pain-generating pathways.

Another technique is using braces, splints, or assistive devices — such as crutches or a cane — to decrease the pressure on the affected area. If allowed, gentle joint motion is better than keeping a joint stiff without movement.
Finally, our mind is a powerful tool in managing pain. Meditation and other mindfulness techniques can help reduce stress, calm anxiety, and regulate the response to pain.
Q: What should young athletes know about sports overuse injuries and how to treat them?

Avoiding overuse means taking periods of rest. This can range from decreasing the time spent practicing the painful activity, to spending more time cross-training, to taking time off from the sport.
Poor technique means that extra stress is inappropriately placed on joints or muscles, leading to pain. Deficits are often seen in joint motion and surrounding muscle strength, which can contribute to poor technique.

If symptoms do not resolve with simple rest or activity modification, or seem to reoccur with greater frequency, then young athletes should be evaluated by a medical professional. Often, these types of injuries can be managed with rest and physical therapy, but it is critical for young athletes to also be evaluated for underlying organic or mechanical issues that may predispose them to these types of injuries.


This unexpected increase in injury is rooted in the idea that for the athlete to reach their full potential, they have to play the same sport throughout the year. The lack of cross-training — young athletes are increasingly specializing early in a single sport — and time to rest and recover from their training has led to injuries associated with overuse and fatigue.
Participating in more than one sport throughout the year allows for the development of other physical attributes and hand-eye coordination, while reducing stress and resting the areas that are prone to injury in specific sports.