Exploring Chicago’s rich history of physician activism
Fact checked by Derick Wilder
The day that physician residents and fellows at Northwestern Medicine voted 794 to 148 to unionize, some shared their joy on social media.
“So proud of the community of residents and fellows who made this happen. Unions increase workers’ democratic voice; raise wages and build wealth; and improve conditions for all workers. WE DID IT,” wrote third-year resident Hebron Kelecha, MD, on X (formerly Twitter).
Northwestern Medicine’s physicians-in-training aren’t Illinois’ first group to unionize (800 residents at University of Illinois Chicago unionized in 2011), but Northwestern’s group is the largest in the Midwest, with almost 1,300 doctors.
While the idea of physicians unionizing is relatively new, activism among physicians isn’t. Physicians regularly advocate for their patients. Many operate under the Hippocratic concept of, “First, do no harm.”
But what if the harm is coming from beyond anything the physician and patient can control, such as from the environment, structural racism, insurance companies’ denial of care, or lack of access to healthy food?
The antibiotic prescribed for a single mother’s urinary tract infection, for example, may be less important to her than finding a job that pays a living wage, securing childcare for her two children, and moving to a safer neighborhood. The hernia repair operation that a laid-off factory worker needs may be less important to him than his lack of health insurance, his need to acquire skills in order to find a new job, and his concern about making rent payments while unemployed.
That’s when a physician might switch from advocacy — working on behalf of an individual patient — to activism, which involves pushing for social and political changes that impact entire communities. Still, if physicians take an oath to do no harm, is fighting the systems that harm their patients considered activism? Or are they simply doing their job?
Twenty years ago, an issue of the American Medical Association’s Journal of Ethics focused on physician activism. In his opening letter, Editor Jeffrey Kullgren wrote, “If we are truly dedicated to improving the lives and well-being of our patients, and if we honestly care enough about the vulnerable persons that have trusted us to care for them, we have an obligation not only to provide health care of the highest quality, but also in some way, shape, or form to be active in public policy changes needed to better their lives.”
Former U.S. Surgeon General Antonia C. Novello, MD, DrPH, embodies that concept. “I loved the practice of medicine, where the focus is on individual patients, but early in my career I realized that my strongest interest is in improving the health of large population groups,” Novello said in an interview in the same Journal of Ethics issue. “I wanted to be able to do something about the major health issues facing people in this country, such as the need to increase access to healthcare for the uninsured, the need to ensure that the healthcare in this country is high-quality care, and the need to improve the health status of Americans through greater emphasis on prevention and healthy lifestyles.”
To address the issues, Novello went from the medical clinic to the political arena. Yet, for many physicians, activism — especially in the wake of Covid-19 — increasingly happens in the clinic and on the streets.
The legacy of Quentin D. Young, MD
Chicago is an epicenter of corporate and political power. It’s a city of health insurance and pharmaceutical companies, and the headquarters for many medical associations, including the American Medical Association. One of the country’s largest safety-net hospitals also calls Chicago home. John H. Stroger, Jr. Hospital (formerly known as Cook County Hospital or more commonly “County”) has attracted and shaped many physician activists, including the legendary Quentin D. Young, MD.

Young believed fervently in healthcare for all — “Everyone in, nobody out!” was his mantra — achievable only through a universal-financing mechanism. Countries typically achieve universal health coverage through single-payer financing. Medicare, for example, is a form of single-payer healthcare; however, it’s not universal health coverage because not all U.S. citizens qualify for Medicare — only those age 65 and over.
The United States is the only high-income country in the world without universal health coverage. While most Americans agree that healthcare is a basic human right, how to finance such care, especially via the government, is as divisive a topic as abortion or politics.
“For Quentin, it was a moral argument,” says Margie Schaps, HMPRG’s executive director since 1993. “He wasn’t a believer in incrementalism. If you want transformative change, small steps will not get you there. And Quentin wanted transformative change.”
The revolution did not happen in Young’s lifetime, but other generations of physicians influenced by his moral argument picked up the mantle.
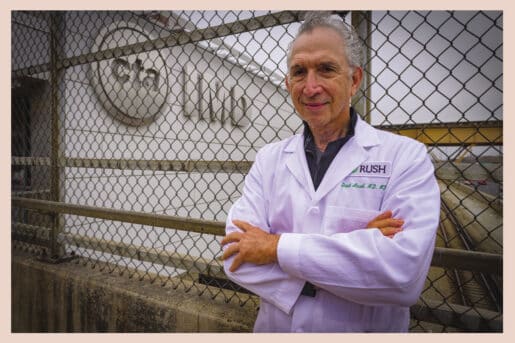
A direct descendant in the physician activist family is David Ansell, MD.
Today’s physician activist leadership
To talk with Ansell is to receive a crash course in the social determinants of health and the industrial healthcare complex. He’s currently senior vice president for Community Health Equity at Rush University Medical Center and associate provost for Community Affairs.
Ansell went to medical school in upstate New York to “do good for people.” But when handed a stethoscope branded by Eli Lilly, he thought about leaving for forestry school.
Unfortunately for the trees, Ansell stayed the course and upon graduation headed to Chicago with one intention: to train under Young, then-chair of medicine at Cook County Hospital.
“I came to Chicago because I was an activist, and I learned how better to be an activist,” Ansell says.
Ansell’s 2011 book, County: Life, Death and Politics at Chicago’s Public Hospital, includes an introduction from Young and chronicles the history of Cook County and his years there.
Activism is part of the social medicine skills that Ansell and co-author Kristen Pallok, MD, describe as key in the 2022 AMA Journal of Ethics article “Should Clinicians Be Activists?” The article also explores reasons physicians may shy away from activism.
Some physicians may consider themselves apolitical, or they view any treatment as better than no treatment. Others might disagree that healthcare is a human right, or fear for their employment. And some physicians don’t think they have the time or expertise for health activism.
Ansell has never been one of those physicians. Rush University leadership tapped him after he’d spent 30 years working at Chicago’s safety net hospitals (more than half at County, the rest at Mount Sinai Hospital) to serve as its inaugural chief medical officer.
I thought, what the heck? It’s across the street,” Ansell recalls.
The view from Rush changed his perspective entirely.
“I understood for the first time how structural racism in health inequities were built into one street,” Ansell says. “There were two worlds, all tied to a capitalist system where White people have better insurance, and Black and Brown people are at the bottom.”
He saw the contrast between those worlds most starkly in organ transplant patients. “In my 30 years at [Cook] County and Sinai, none of my patients ever got a life-saving organ transplant. But the organs transplanted into White patients all came from Black and Brown bodies.”
Achieving equity
While demonstrating via sit-ins and marches can be an effective form of activism, using research to take on a system and force it to change is especially powerful. Under Ansell’s direction, Rush became one of the first hospitals in the country to establish health equity as a system strategy and measurable organizational priority.
Ansell believes that an increasing number of medical students come to Rush because of this strategy. The health equity and social justice leadership course is often oversubscribed, but medical students train across all curricula in anti-racism and health equity.
And for Ansell, universal healthcare offers a direct path to more equitable healthcare.
“The nature of our health system perpetuates this inequity that puts Black and Brown people at the bottom of the pile; it’s a caste system. Single-payer, or something like it, where everyone gets the same card at birth, will improve outcomes for the population,” he says, adding, “But that’s not enough.”
Physicians for a National Health Program (PNHP) advocates for universal, comprehensive single-payer national health insurance, joining with other organizations to fight racism and advance social justice. Founded in 1987 in Cambridge, Massachusetts, by Steffie Woolhandler, MD, and David Himmelstein, MD, the program moved its headquarters to Chicago in 1991. The city’s strong activist cohort that included physicians Young, Gordy Schiff, MD, and Claudia Fegan, MD, made the new home appealing.
Susan Rogers, MD, the immediate-past-president of PNHP, spent most of her clinical career as an internist at Stroger Hospital. She currently serves on the faculty of Rush University and its medical school admissions committee.
Rogers grew up in Hyde Park “which was so totally integrated, I never knew there were all-White or all-Black neighborhoods,” she says.
In 7th grade, her mother took her and her two siblings to march with Martin Luther King, Jr., to protest school segregation. “It was then I realized how awful things were. My mother was pushing this, so I thought, this must be important.” At the brand-new Kenwood High School, as the Vietnam War was escalating, “that’s when I had a sense of using my voice to protest for change.”
As a Black student at the small western college that Rogers first attended, she “wasn’t exactly welcomed,” so she returned to Chicago to study biology at Roosevelt University. Unsure of whether she wanted to be a teacher, nurse, or doctor, she went on to graduate from medical school at the University of Illinois.
Rogers loved being an attending at Stroger Hospital. “I went to County to take care of Black people. That is part of my activism.”

Educating doctors in activism
Now, Rogers and the Rush admissions committee look for a wide array of applicants. Some of them have volunteered locally or globally, and many are attracted to Rush because of its affiliation with Stroger Hospital.
That said, Rogers notes the lack of Black physicians in the U.S., which correlates with the demographics of medical school applicants. Per Rogers, most applicants come from families with incomes in the top 20%, and many are children of physicians.
Rogers attributes much of the inequality in health outcomes to income inequality and to institutionalized racism.
“Because this country is so segregated, people don’t grow up really knowing people who did not grow up like them,” she says.

Verhoef moved to Chicago to get additional training in critical care at the University of Chicago Medicine. “That is really when I became activated in the single-payer movement. PNHP was based in Chicago, and there were a lot of activists,” he says.
Now, though, Verhoef says he understands why younger physicians might avoid activism. Sometimes saddled with hundreds of thousands of dollars of debt, just starting their practices or families, they have neither time nor energy for activism. That lack of resources also applies to physicians on the front lines of inequity in emergency rooms, trauma centers, and safety-net hospitals.
While an event sparks some physicians into activism — such as the Flint, Michigan water crisis, exposed by a pediatrician — Verhoef sees himself as an educator for activists, through his role with PNHP. “Students don’t know the system they’re getting into.”
Like Ansell, Verhoef says that activism requires a certain skill set. “Let’s teach [doctors] how to be an activist, not just an advocate, because it’s part of your professional identity.
We are at the top of the food chain, and people listen to us.”
The medical residents and fellows at Northwestern University’s Feinberg School of Medicine experienced just how powerful their voices can be when they secured unionization.
Verhoef says he sees clear benefits in their action. “We built many of our hospitals to function on the backs of resident labor, ripe for exploitation. Why do we work as much as we do and have no say in this process?”
Yet, he says, there’s more work ahead. “We need to start using our voices to get the healthcare we want and deserve in this country. That is our moral obligation as healthcare professionals.”
More physicians than ever, it seems, are doing exactly that.











