Treatments offer men relief for a common uncomfortable condition
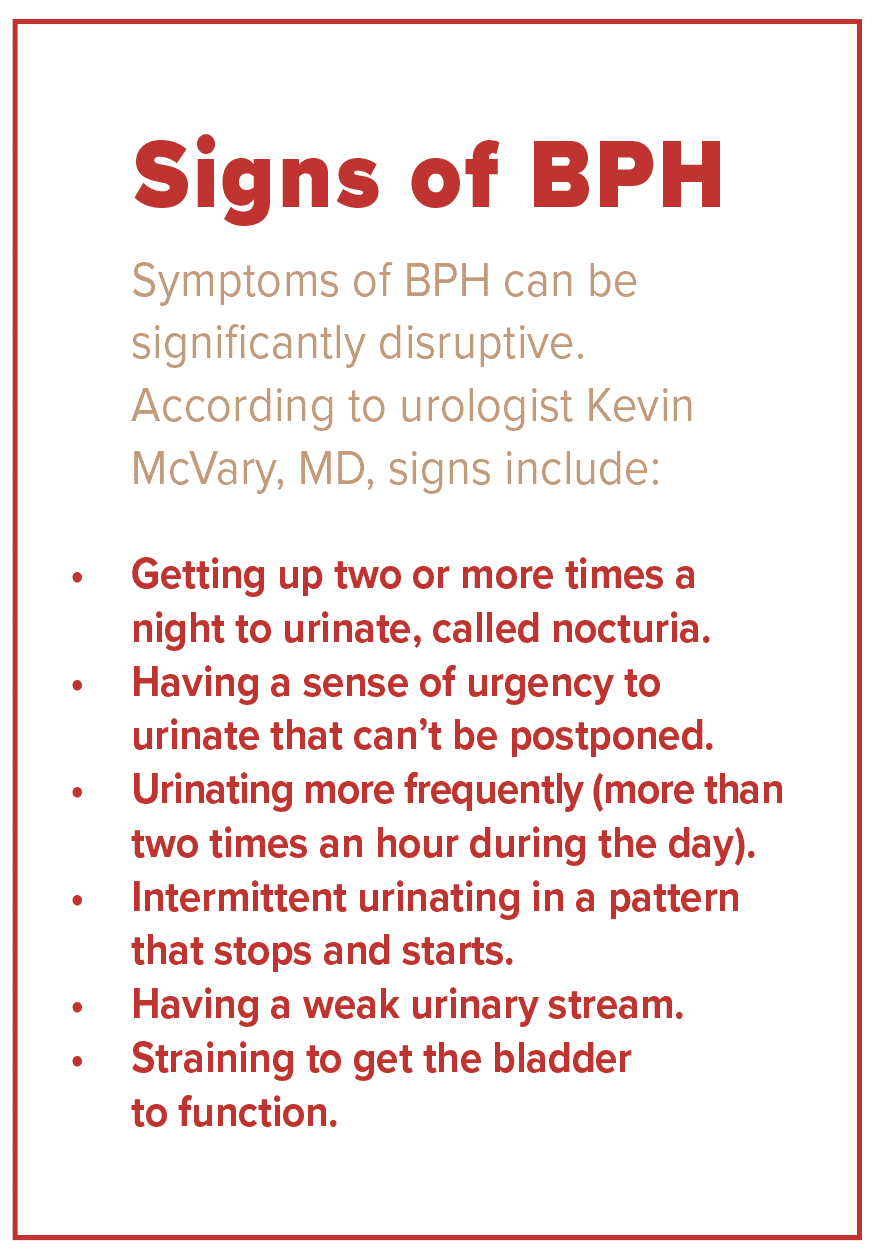
About 10 years ago, Steven Prosser, of Libertyville, started beating a path from his bedroom to his bathroom five or six times every night to urinate. His problem got progressively worse until Prosser, who is now 57, was waking up more and more often to go to the bathroom and then wasn’t falling asleep afterward.
The issue continued throughout the daytime, too. He’d go to the bathroom right before he left home for his 75-minute commute to work. Sometimes, he even had to make a restroom stop on the way there. During meetings, he’d have to make a couple of trips to the men’s room.
“I’d go to the restroom, and, five minutes later, I would feel as though I had to go back because I could never empty my bladder,” he says. “If I held off from going to the bathroom, I’d have to work hard to start up, push to get started, and I’d get very little out. My day revolved around the restroom.”
Prosser’s experience will sound familiar to many. It is the result of a common, noncancerous condition called benign prostatic hyperplasia (BPH), which can result in lower urinary tract symptoms.
The prevalence of BPH increases steadily with age. The older you become, the more likely you are to be diagnosed with it. The condition affects 50% of men between the ages of 51 and 60. By the time they hit 80, 90% of men have BPH.
The cause of BPH isn’t known, although in some men it may be hereditary. Prosser’s late father had BPH, as do two of his brothers.
Prostate changes
BPH symptoms occur when a portion of the walnut-size prostate gland progressively grows new tissue as men age.
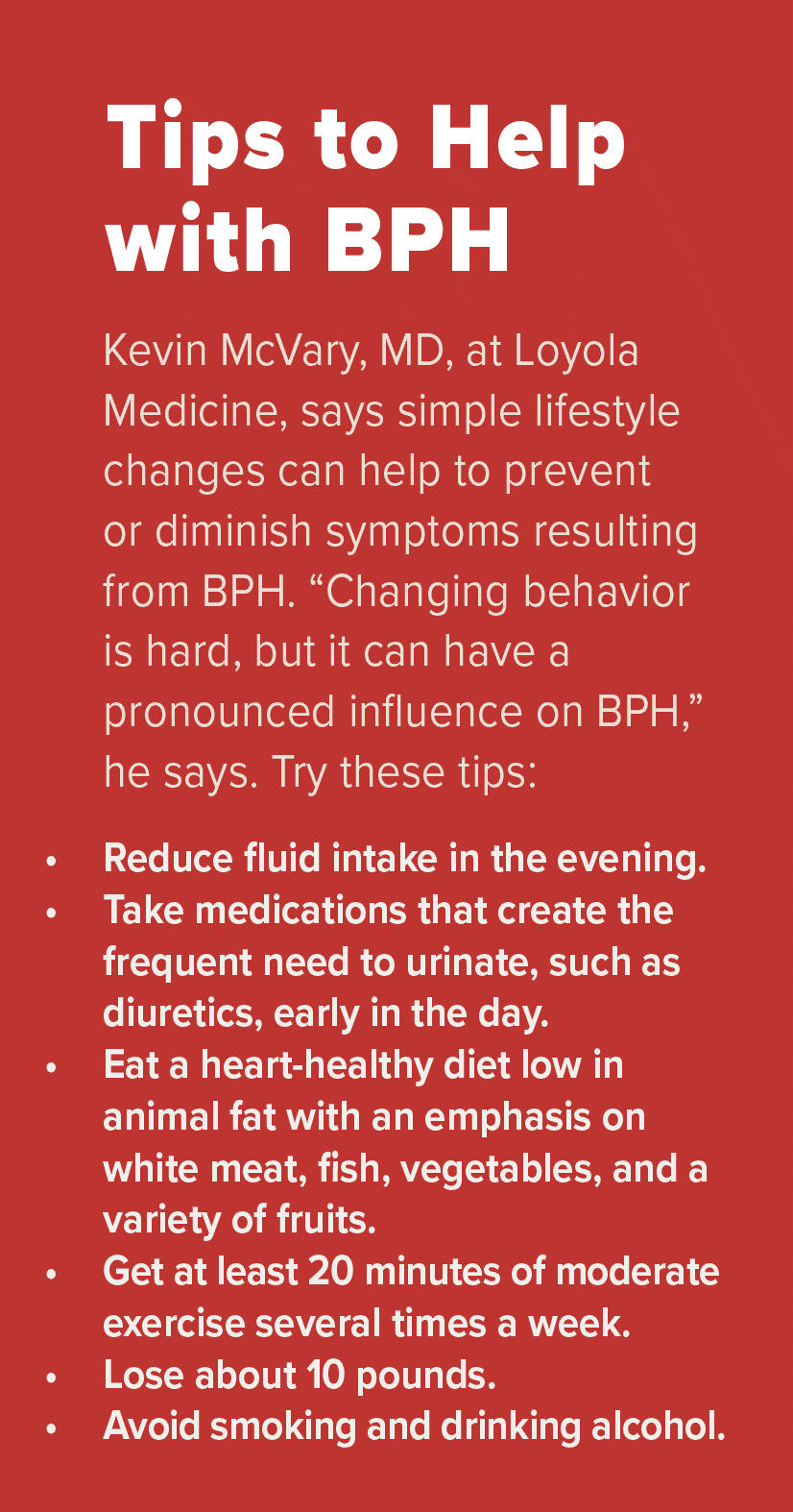
“As the prostate enlarges, it begins to crimp and compress the urethra, the canal that runs through it from the bladder and allows urine to leave the body when men urinate,” explains Kevin McVary, MD, a urologist at Loyola Medicine and director of the recently opened Men’s Health Center at Loyola. “When the prostate clamps down tighter and tighter on the urethra, the bladder, in response to this obstruction, starts to become a stronger muscle, increases its power, and continues its march toward obstructing the urethra.”
This development interrupts the urination pattern. “The bladder loses the war, and the prostate wins,” McVary says.
In diagnosing BPH, physicians review a person’s medical history and conduct a physical exam. The American Urological Association’s BPH symptom score index helps physicians determine severity.
“I’d go to the restroom, and, five minutes later, I would feel as though I had to go back because I could never empty my bladder.”
“This allows us to somewhat objectively quantify if the symptoms are mild, which might simply require active surveillance, to moderate or severe,” says Richard Harris, MD, a urologist and director of the UroPartners prostate cancer centers.
Doctors may also use tests that measure the amount of urine left in the bladder after urination and a uroflowmetry test to measure how fast the urine flows when a man urinates.
Treatment options
If left untreated, BPH may lead to bladder damage, urinary retention, blood in the urine, a urinary infection, and even kidney damage, Harris says.
Physicians typically begin by pre- scribing alpha-blockers — medications that relax the muscle of the prostate and bladder neck. These medications, usually taken long-term, typically improve the flow of urine within a couple of weeks. However, “They don’t work for everyone and can have a negative influence on sexual function,” McVary says.
Additionally, men may take 5-alpha reductase inhibitors to shrink the prostate. These medications can take up to six months to increase urinary flow and must be taken indefinitely. “They are only helpful in about 20% of men, and there is a risk of erectile dysfunction,” McVary says.
Surgery is another option. Trans-urethral resection of the prostate (TURP), performed in a hospital under anesthesia, uses an electrical loop to cut away the prostate tissue and seal blood vessels.
“While it is still considered the gold standard for prostate surgery, the number of TURP surgeries has been greatly reduced as the number of newer procedures have been developed,” Harris says.
Newer treatments include a minimally invasive procedure that uses an implant to lift and hold the enlarged prostate so it no longer presses on the urethra, thus enabling the urethra to open up and function normally.
Another FDA-approved minimally invasive option uses water vapor therapy. During this procedure, performed in the doctor’s office under anesthesia, physicians insert a tiny telescope into the urethra and use a retractable needle to inject a small amount of water vapor. The steam kills the part of the prostate tissue blocking the urethra. “It takes only 10 minutes,” McVary says. “Men can come off of medication, and there is no risk to sexual function.”
McVary recently published a study in the Journal of Urology reporting that the water vapor procedure continued to offer significant improvements in lower urinary tract symptoms and flow rate, as well as quality of life, for at least five years for the vast majority of men who have the procedure.
Prosser, who previously passed out from one of his BPH medications that can cause dizziness and low blood pressure, underwent the water vapor procedure last summer. “It was painless. The only problem is that you have to be catheterized for two days afterward, which is uncomfortable,” he recalls.
With a variety of treatments now available, men with BPH should consult with a doctor to find the best option to relieve their symptoms.
The procedure made a huge difference for Prosser. “Now it’s not uncommon for me to go an entire night without waking up, and I’m more rested during the day. I know that when I go, I empty my bladder every time,” he says. “I no longer have to run my life around going to the bathroom.”
Originally published in the Spring/Summer 2021 print issue.

Nancy Maes, who studied and worked in France for 10 years, writes about health, cultural events, food and the healing power of the arts.












