Planning for hospital discharge
Hospital discharge — the process when a patient heads home after a hospitalization or procedure — brings a sense of relief for some, a moment to celebrate for others, and a time fraught with problems and worry for many.
No two discharge experiences are alike, due to so many moving parts, says Teri Dreher, nurse, author of Patient Advocacy Matters, and founder of patient advocacy company NShore Patient Advocates.
“At times, discharges are very rushed because hospitals have a shortage of nurses and physicians. Patients may be discharged too soon because health plans only cover a certain number of days, or hospitals need the beds,” Dreher says. Additionally, she adds, problems crop up because many patients or their loved ones “don’t read the discharge papers and are not prepared to care for the patient at home.”
Frankfort resident Mary Kay Doyle remembers the discharge procedure when her husband, Brian Doyle, 65, a retired fire fighter and paramedic, was in the hospital for neck surgery. The nurse releasing Brian from the hospital waited for Mary Kay to arrive to talk through Brian’s instructions for home, which Mary Kay appreciated.
However, the discharge paperwork was 12 pages long. To Mary Kay’s relief, the nurse wrote down key information, including when Brian last had pain medication and when he should get the next dose. “I wasn’t going to remember that when I got home,” says Mary Kay, 62, who works part-time as an administrative assistant. “Sometimes I can’t even remember where I put my car keys.”
Mary Kay’s reaction during the discharge process is common, Dreher says. “People are stressed out, and the patient may be in pain during the discharge. The information may not be sinking in, so they may think they will remember it, but they don’t.”
When preparing to leave the hospital, people often worry about their own responsibilities and abilities as a caregiver. Putting a plan in place can make the transition easier on the patient and the caregiver.
“People are going through a repetitive loop of emotions, worrying what life will be like at home after the discharge, so it’s important for them to write information down in a notebook or type it on their phone,” says Wendy Benson, chief operating officer of 2 x 2 Health: Private Health Concierge and co-author of The Confident Patient.
Include the names and contact information of all the medical professionals involved in the person’s care, as well as expectations for the healing process. If the patient’s family members live far away, one of them could ask to be present during discharge by telephone, Benson says. A friend or neighbor could also attend the discharge.
“We feel comfortable asking a member of the wait staff in a restaurant about the ingredients in a sauce, but not asking a doctor to explain something that isn’t clear. There are no silly questions.”
Benson suggests asking to see discharge instructions in advance, even in draft form, so the patient and family caregiver can formulate questions they want to ask and make plans, such as scheduling follow-up appointments.
The discharge papers offer a lifeline to a safe recovery. Mary Kay says that when Brian returned home, he started vomiting. His discharge instructions recommended contacting his surgeon. Thinking she might be over-reacting and wasting the doctor’s time, Mary Kay instead called the private health advocate she had been working with, who encouraged her to call the doctor. It was the right thing to do. The surgeon quickly readmitted Brian to the hospital.
“Don’t ever be afraid of taking up a doctor’s time, as that’s what they are there for,” Benson says. “We feel comfortable asking a member of the wait staff in a restaurant about the ingredients in a sauce, but not asking a doctor to explain something that isn’t clear. There are no silly questions.”
Questions for a Safe Discharge from the Hospital
Clip this list, and bring it to your or a loved one’s next hospitalization.
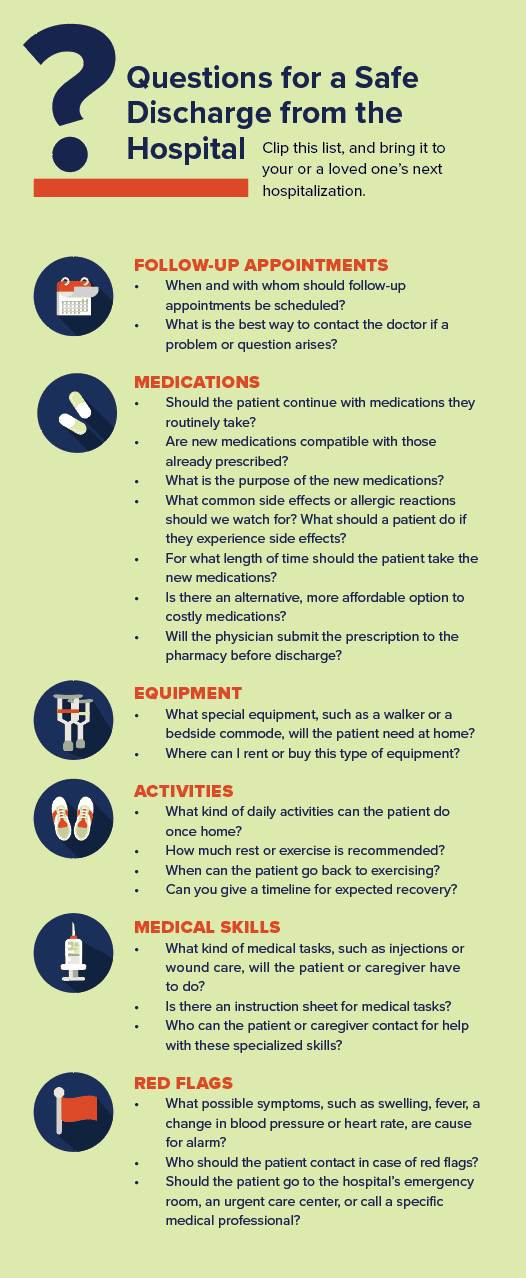
FOLLOW-UP APPOINTMENTS
- When and with whom should follow-up appointments be scheduled?
- What is the best way to contact the doctor if a problem or question arises?
MEDICATIONS
- Should the patient continue with medications they routinely take?
- Are new medications compatible with those already prescribed?
- What is the purpose of the new medications?
- What common side effects or allergic reactions should we watch for? What should a patient do if they experience side effects?
- For what length of time should the patient take the new medications?
- Is there an alternative, more affordable option to costly medications?
- Will the physician submit the prescription to the pharmacy before discharge?
EQUIPMENT
- What special equipment, such as a walker or a bedside commode, will the patient need at home?
- Where can I rent or buy this type of equipment?
ACTIVITIES
- What kind of daily activities can the patient do once home?
- How much rest or exercise is recommended?
- When can the patient go back to exercising?
- Can you give a timeline for expected recovery?
MEDICAL SKILLS
- What kind of medical tasks, such as injections or wound care, will the patient or caregiver have to do?
- Is there an instruction sheet for medical tasks?
- Who can the patient or caregiver contact for help with these specialized skills?
RED FLAGS
- What possible symptoms, such as swelling, fever, a change in blood pressure or heart rate, are cause for alarm?
- Who should the patient contact in case of red flags?
- Should the patient go to the hospital’s emergency room, an urgent care center, or call a specific medical professional?
Originally published in the Fall 2022/Winter 2023 print issue.

Nancy Maes, who studied and worked in France for 10 years, writes about health, cultural events, food and the healing power of the arts.












