Helping women with endometriosis find relief
Endometriosis is a women’s health issue that has long remained in the shadows. Even though the condition can cause intense pelvic pain, it’s often overlooked, with symptoms chalked up to menstrual discomfort.
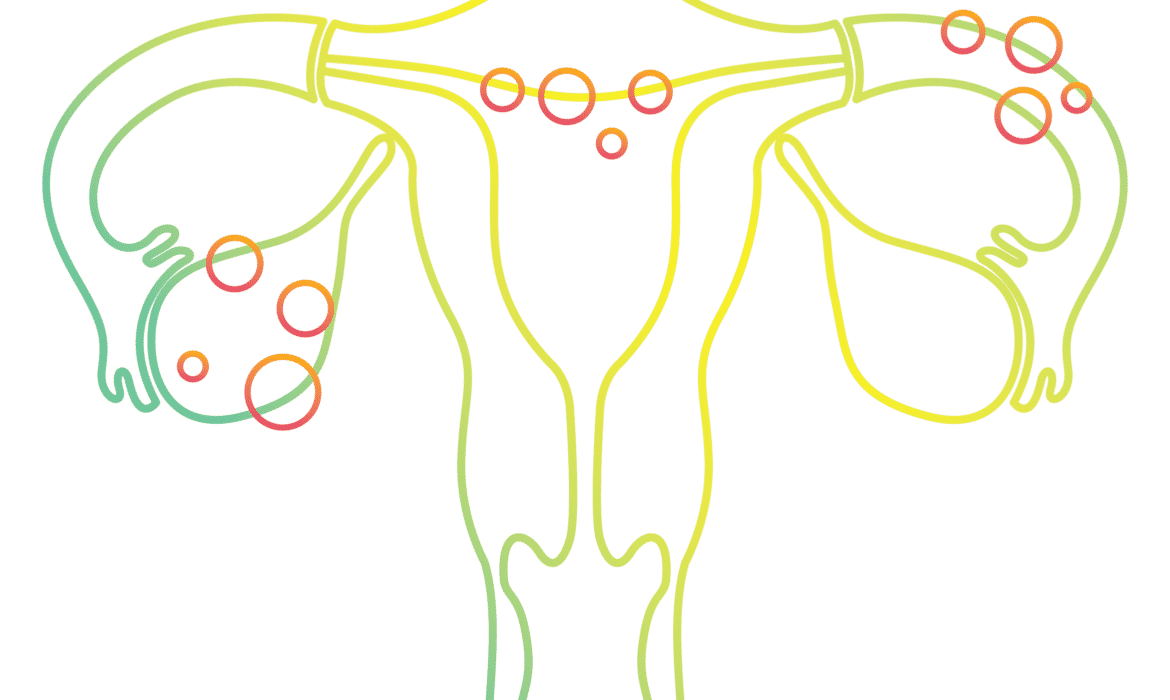
Many doctors are not well-trained in this chronic condition, which occurs when cells similar to those inside the lining of the uterus escape and grow outside of their normal location. As those cells grow, cysts and scar tissue can form. Many women suffer for a long time without relief, on average waiting almost 7 years to get a diagnosis, according a study in the journal Fertility and Sterility.
The experience of Evanston-resident Jessica Cooper, who asked that her real name not be used, highlights the problem. Around age 15, she started having very irregular periods with heavy bleeding and severe pain. “I was put on continuous birth control that [stopped] working after a while,” she says. “So I was switched to different meds, beginning with a low-dose hormone treatment.”
Despite starting treatment at a young age, Cooper required abdominal surgery in her early 30s to remove two large cysts on her ovaries. “The cysts were causing a lot of pain and were deemed related to endometriosis,” she says. “That was the first time I heard that word.”
Identifying symptoms
Cooper’s situation is not uncommon. Endometriosis affects at least 11 percent of American women between the ages of 15 and 44, according to the U.S. Department of Health & Human Services. Endometrial tissue commonly spreads to the ovaries, the fallopian tubes, the outer surface of the uterus and the tissues that hold the uterus in place. It also may grow on the vagina, cervix, vulva, bowel, bladder or rectum.
“Sometimes the symptoms of women having menstrual complaints are disregarded or dismissed as a normal part of being female, or women get an inappropriate diagnosis that can cause a delay in the initiation of the appropriate treatment,” says Linda Yang, MD, a minimally invasive gynecologic surgeon at Loyola Medicine. But early diagnosis is important when it comes to receiving appropriate treatment.
While the exact cause of the condition is unknown, Yang says it might be the result of an immune disorder or menstrual blood flowing back through the fallopian tubes. Symptoms include pelvic pain — often severe — during the menstrual cycle and at other times, too. Women may also have spotting or bleeding between periods, as well as digestive problems such as nausea, constipation or diarrhea, painful bowel movements or pain when urinating or during intercourse.
It can also cause infertility.
Getting treatment
Women with endometriosis may also suffer from additional health issues, such as irritable bowel syndrome and chronic bladder problems. This can make it difficult to get a correct diagnosis.
“It’s a real challenge to diagnose endometriosis because you have to ask questions about symptoms beyond the reproductive organs, and if the patient has other issues you ideally want to treat those too,” says Frank Tu, MD, MPH, division director for gynecology at NorthShore University HealthSystem.
A physician with expertise in endometriosis can diagnose the disease by feeling the thickened nodules of the condition in the pelvic area during a physical exam in younger women. It can be more difficult to diagnose an older woman this way, since thickened nodules may suggest something else, such as cancer.
Endometriosis is a women’s health issue that has long remained in the shadows.”
While there is no cure for endometriosis, a variety of medications are available to manage the symptoms. Painful cramps can be treated with over-the-counter drugs such as Advil and Aleve, as well as muscle relaxants. Hormonal birth control methods can be prescribed to lower the level of estrogen in the body. Among other options is a drug that decreases estrogen to the levels of menopause, a process that can be reversed when the woman stops taking the medication.
If medications are not effective, a minimally invasive laparoscopic procedure can be performed in which a small camera is inserted through the abdomen to look for endometriosis lesions outside the uterus and determine if they should be surgically removed. Surgery itself, wherein the endometrial tissue and any associated scar tissue is removed, gives women significant, immediate relief, Tu says.
In extreme situations, a hysterectomy may be recommended. That was the case for Cooper, who had worsening pain and bleeding after her cysts were removed. She was diagnosed with adenomyosis (when endometrial cells grow into the uterine wall), in addition to endometriosis. Cooper consulted with Tu, who performed the surgery in January 2018 to remove her uterus and cervix, leaving her ovaries intact.
“When I was in my 30s, I wanted to preserve my fertility. And at 42, I still want to have kids but I’m comfortable with other ways of doing that,” Cooper says. “The improvement in my quality of life has been tremendous, and I have so much more energy.”
In addition to medical treatments for women with endometriosis, Tu recommends lifestyle changes. He suggests a Mediterranean diet, exercise, stress management and physical therapy of the pelvic floor to help manage uncomfortable symptoms.
Tu is involved in the fifth year of a study that seeks to better understand factors in young women with painful periods (common in endometriosis). Researchers hope to predict who is likely to develop chronic pain and determine if early treatment of period pain can prevent chronic pain.
Women need to learn more about pelvic health and endometriosis so they can recognize symptoms early.
Tu says it’s important to educate young girls so they know when their menstrual health is not normal and to have period pain treated early so it doesn’t worsen.
After her own experience, Cooper has advice for other women: “You know your own body. If something doesn’t feel right, speak up and be your own advocate.”