How Chicagoans have historically shaped, and continue to transform, healthcare
Fact checked by Derick Wilder
Our story begins 160 years ago, during the Civil War era. Elizabeth Blackwell, MD, the first woman to earn a medical degree in the U.S., had graduated only 15 years earlier, in 1849. Blackwell was exceptional; most institutions at the time barred women from higher education and professional work. With a few exceptions, women largely couldn’t vote, take legal action, or own property.
Life looks vastly different for women in the U.S. now, though many states have banned access to sexual and reproductive medical care for women. And while more women are practicing medicine today, they remain devalued among their male counterparts by nearly every metric and measurement, including pay equity and leadership roles.
“Getting consultants and patients to believe that I, as a young woman, hold the same amount of knowledge as someone more senior-appearing and masculine-presenting is often challenging, regardless of how many times I assure them that I am indeed a physician,” says Nikki Alberti, MD, an emergency and internal medicine resident at the University of Illinois Chicago. “I truly believe that as the number of women in medicine continues to rise, this culture change will happen.”
Today, about 36% of physicians nationwide are female. Data show that they are transformational leaders and that their patients have lower readmission rates and fewer complications in surgery. Most women physicians choose specialties that focus on women and children (pediatrics, obstetrics and gynecology, and adolescent psychiatry). The numbers will continue to shift, however, as 2019 marked the first time in the U.S. that women outnumbered men in medical school, making up 50.5% of enrollees.
Unfortunately, the healthcare system was largely built before women were allowed to participate in the field, which means they rarely had any voice in its development. But, women in Chicago have a history of making big changes. Here’s a look at just a few of them — starting with the landmark women of decades past and their counterparts in today’s women in Chicago medicine.
Transforming systems
Mary Harris Thompson, MD, and Shikha Jain, MD
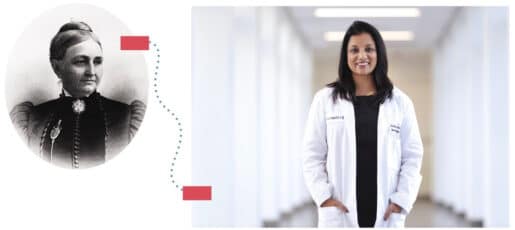
The city of Chicago had existed for only 30 years when Mary Harris Thompson, MD, arrived in the mid-1860s from Boston. She had attended medical school at the New England Female Medical College, studying under Blackwell.
In Chicago, Thompson cared for Civil War veterans’ families, but she was limited in what she could do because hospitals in the city banned women doctors from practicing; one hospital wouldn’t even admit women as patients.
So Thompson took matters into her own hands. In 1865, with community fundraising, she established the Chicago Hospital for Women and Children. Thompson served as chief surgeon and head of staff.
Five years later, she co-founded the Woman’s Hospital Medical College. When Northwestern University absorbed the school in 1892, Thompson served as a professor of gynecology until her death in 1895 from a brain hemorrhage.
Harris’ commitment to women physicians lives on today in Shikha Jain, MD, associate professor of medicine in hematology and oncology and director of communication strategies in medicine at the University of Illinois Chicago. Only now, instead of fighting to practice medicine, women physicians are advocating for leadership roles and equal pay.
Since 2019 and 2021, respectively, Jain’s Women in Medicine Summit and nonprofit, Women in Medicine, have elevated women’s voices and matched young medical students with mentors. “We have come a long way in addressing the inequities that exist in our healthcare workforce. Several decades ago, these topics were not even discussed, but now they have become a part of our national dialogue,” Jain says.
Jennifer Laflamme, DO, works in psychiatry at Advocate Lutheran General Hospital in Park Ridge. She says she hopes to see more women in medical leadership roles.
“In my experience, the female attendings that I have precepted with are often the most detail-oriented, patient, compassionate, and thorough when it comes to patient interactions and teaching,” Laflamme says. “I think their unique perspective and skill set lends itself well to leadership.”
She says she also hopes for more recognition of family planning and family leave time. “As a resident and mother of two children, I am keenly aware of the challenges associated with working hard to advance in a career in medicine while also balancing the demands of growing a family.”
Data confirms that gender bias still exists, and the makeup of medical leadership, salaries, and awards reflects that bias. Studies show these disparities directly impact community health. “More organizations and systems are making an effort to understand these disparities and work on addressing them. But we are a long way from equity, and there is much work to be done,” Jain says.
Jain’s passion grew out of the personal struggles and barriers she encountered in the medical field. Conversations with peers illustrated that her experiences were a common narrative among women in medicine. She set out to change that narrative.
The Women in Medicine Summit has grown significantly since 2019, with more than 500 people in attendance last year. “We know that we are all stronger together and can drive real systemic change together, as we grow our networks, empower women and allies, and strategically work towards positively disrupting the system,” Jain says.
And as Harris did during her time, Jain pushes for equity. “The health of our communities depends on it,” she says.
Reshaping healthcare and social welfare
Jane Addams and the Jane Addams Senior Caucus
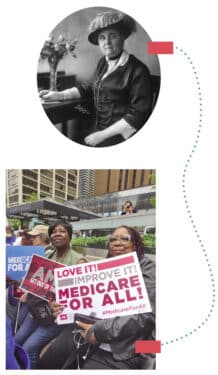
Not long after Harris took on women’s access to healthcare in Chicago, Jane Addams emerged as a leading force for under-resourced communities. Born in 1860, in Cedarville, Illinois, Addams became a revolutionary figure in healthcare reform and social work.
Recognizing the dire need for social services, particularly in healthcare, Addams, along with social reformer Ellen Gates Starr, established Hull-House in 1889, a settlement house that became the cornerstone of her efforts to address the health disparities plaguing Chicago, such as poor sanitation, childhood malnutrition, and healthcare access for immigrants and people living in poverty.
Addams believed in a holistic approach to social reform.
She and other volunteers provided medical assistance, health education, and sanitation resources to impoverished residents. And Hull-House built the first public playground in Chicago, emphasizing the link between physical activity and overall well-being.
Addams also focused on combatting tuberculosis (which she’d had as a child), and those efforts demonstrated her ability to mobilize resources and influence policy. That influence paved the way for national healthcare reform movements, including the establishment of Medicaid and Medicare in the mid-1900s.
Addams’ impact remains evident in Chicago’s healthcare landscape. Hull-House inspired a wave of social service agencies and healthcare facilities, including the Jane Addams School of Social Work on the University of Illinois Chicago campus and the Jane Addams Senior Caucus. These organizations continue to follow Addams’ lead and serve vulnerable communities. The caucus, founded in 1976, advocates for vulnerable seniors and campaigns for better medical and healthcare policies, as well as economic, social, and racial justice.
For example, in response to heat-related deaths in a senior living facility in 2022, the caucus successfully campaigned for changes to the city’s municipal code, requiring relief for residents during extreme heat events. Their focus extends to housing campaigns, addressing issues in Section 8 senior buildings.
Whether it’s replacing 30-year-old carpet or removing asbestos, the caucus works in support of better living environments. “Often the living conditions that [tenants] deal with exacerbate the medical issues that they already have,” says Emily King, caucus development director.
The caucus also partners with organizations such as Beyond Legal Aid to help seniors who cannot get medical care due to insurance claim denials.
“Jane Addams charted a North Star for us — the idea that every person has a role to play in the fight for a world where everyone can age with dignity,” King says.
Although Addams passed away in 1935, her legacy endures. Her commitment to social reform, healthcare equality, and the well-being of the underserved has influenced many, including social worker Anuja Martinez, whose volunteer work for a women’s shelter during college steered her toward a career in social work. Today, Martinez works as a social work lead in the adult and children’s emergency rooms at UChicago Medicine, where she regularly meets with survivors of violence, torture, and elder or child abuse.
Martinez says her focus on immigrant needs and holistic wrap-around services comes from Addams’ influence. “[I’m] not just addressing medical needs, but also seeing a person as a complex network of experiences, traumas, and defining moments.”
As healthcare continues to be a focal point of societal discussions, Addams’ vision for a more equitable and compassionate system remains a guiding light for those dedicated to improving the health and well-being of all people.

Revolutionizing research
Janet Rowley, MD, and Funmi Olopade, MD
Fast forward to the 1970s, when women could practice medicine freely, but male physicians outnumbered them 12 to 1 in the U.S. Women were even less common in other areas of science, comprising 38% of the workforce but only 8% of STEM workers.
Janet Rowley, MD, was one of the 8%, and her work changed the world. She attended medical school at the University of Chicago in the 1940s. When she first applied, the quota had already been filled, so she filled the nine months waiting for her turn with other classes.
Rowley started out as a physician but soon switched to research. By the early 1970s, she was raising four sons and working part-time as a cancer researcher at UChicago. Her research focused on leukemia, and she used a rare technique to photograph the cells’ chromosomes under a microscope.
One day in 1972, while analyzing the chromosomes on her dining room table, she noticed something unusual in their structure. Two of them were switching parts of themselves — translocating — to create two mutant chromosomes.
Rowley, the first to observe the action, argued that the swap was creating a genetic mutation that was driving patients’ leukemia. Her discovery eventually translated into Gleevec — a first-of-its-kind, life-saving cancer drug — and changed the way cancer is treated to this day.
At the time, few believed that Rowley was correct. She persevered, making more discoveries, pleading her case at scientific meetings, and publishing her findings in industry journals.
It took decades, but today scientists have linked hundreds of translocations to various cancers, and pharmaceutical companies have used those findings to develop therapies.
“Janet spent her life convincing the medical community that this was important, and no one accepted or believed it,” says Olufunmilayo Olopade, MD, a world-renowned breast cancer researcher and professor of medicine and human genetics at UChicago Medicine.
Olopade knows Rowley’s story intimately, because she started her research in the 1980s in Rowley’s lab.
In Rowley, Olopade saw a passionate scientist who was also a dedicated mother and mentor — an example of what Olopade herself could become.
Olopade came to the University of Chicago looking for a challenging problem, and Rowley advised her to choose one of two paths. “She said I should either learn a skill and become good at it, or focus on a disease area and become the person with the world’s knowledge on this narrow area.”
Olopade chose solid tumors, specifically aggressive breast cancers in Black women, a population long underserved in the U.S. medical system. When researchers linked the BRCA1 gene mutation to breast cancer in 1996, Olopade advocated for everyone to get tested for it. “If we identified at-risk carriers before they developed cancer, we would definitely prevent a lot of disease,” Olopade told the journal Disease Models and Mechanisms in 2021.
The genetic community rallied against her. They were concerned about the cost of testing, as well as the lack of a curative treatment and genetic counselors. They compared the BRCA1 test to being tested for Huntington’s disease (which has no cure).
Olopade staunchly disagreed. “We can cure a lot of cancer if we find it early,” Olopade said in the interview. “I absolutely fought against the genetics community, arguing that this [BRCA1-driven breast cancer] is not like Huntington’s. We can prevent cancer, and it was easy for me to see the path from testing to prevention.”
Similar to Rowley, the disputes urged Olopade forward. “The scientific environment that Rowley inherited from her mentors, from her husband [also a physician scientist, and featured in the next story] — that was the biggest thing that made me motivated,” Olopade says.
And she has advice for scientists starting out now. “Find what really motivates you, and find a role model and mentor that is accessible to you, like the late Dr. Rowley was to me. Inter-generational mentorship is so important. Because, my goodness, the future is so bright.”













