Allergies may be here to stay, but they can be kept in control
Following a pretty brutal winter and a slow-to-start summer, Chicago is finally enjoying some nice weather. Warmer temperatures provide an opportunity to get out of the gym and run or bike along Lake Michigan or perhaps a trail in one of Chicagoland’s many beautiful forest preserves. Each spring brings Midwesterners relief from the darkness and cold of winter. But for thousands of Chicagoans and millions more across the United States, it rejuvenates an old enemy as well.
Allergies.
According to the National Institute of Allergy and Infectious Diseases, 40 to 50 million Americans are affected by allergies. And a nationwide survey found that more than half of U.S. citizens test positive to one or more allergens. How can so many people be so adversely affected by substances that are relatively harmless to many others?
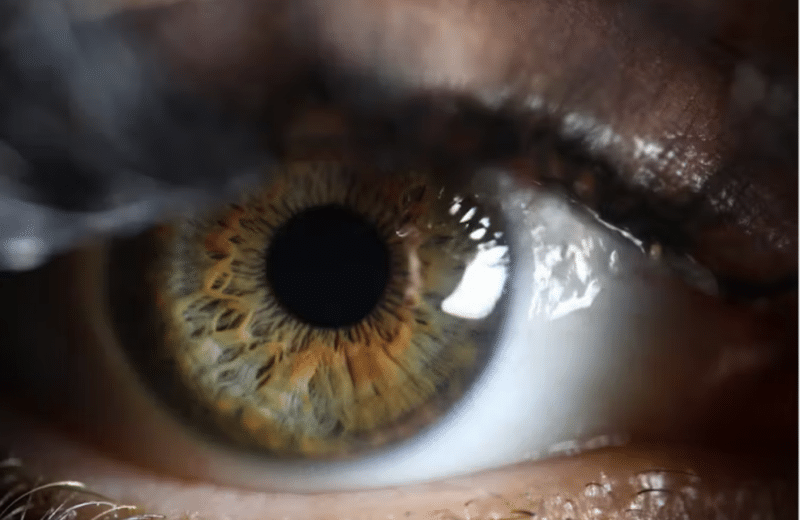
The secret is in the immune system. In people with allergies, their immune systems respond to the presence of normally harmless things like pollen, as if it were a dangerous invader, producing large amounts of the antibody immunoglobulin E (IgE). IgE is the only type of antibody that attaches itself tightly to tissue cells, called mast cells, and white blood cells called basophils. When a pollen allergen comes into contact with an IgE the body has specifically designed for it, they attach. This activates the mast cell to which the IgE has attached, causing it to release chemicals like histamine, resulting in inflammation and discomfort for the allergy sufferer.
The prevalence of several allergies, particularly food allergy and asthma, is on the rise in the United States.
“It’s the million-dollar question as to why that is,” says Dr. Mary C. Tobin, director of the Section of Allergy and Immunology at Rush University Medical Center. There are a few theories. It may be due to an overexposure to antibiotics early in life that has “changed the bacteria in [a person’s] body to a more virulent bacteria, a bacteria that is harder to control and, therefore, his or her system is more permeable,” says Tobin. “So, more protein is absorbed.
“There are some important bacteria in our systems, especially in the gut, that are helpful for maintaining our balance. And sometimes illness [or medication], especially heavy-duty anti-biotics, can interfere with this,” she says.
There is another popular theory as well. Tobin explains: “We are not exposed to enough bacterial proteins early on; we’re too clean. This is the hygiene hypothesis.”
One of the most prevalent allergies, allergic rhinitis, commonly called hay fever, affects between 10 percent and 30 percent of all adults and as many as 40 percent of all children. While the prevalence of rhinitis may not be increasing greatly, scientists warn that climate change could make symptoms worse. In Chicago, climate change will contribute to a longer and warmer spring, leading to higher pollen counts. This is bad news for spring allergy sufferers. In a way, we lucked out with our chilly spring.
“I think we saw that a lot last year,” says Tobin. “It was one of the worst pollen seasons we’ve had from spring to fall.”
The cost of treating rhinitis has risen dramatically as well. The Agency for Healthcare Research and Quality found that from 2000 to 2005, the cost nearly doubled—up from $6.1 to $11.2 billion. More than half of this cost is attributed to prescription medications.
Why are some folks left unable to function without daily medication, while others have only a minor case of the sniffles? One factor is genetics.
“You get allergies because at least one of your parents has allergies,” says Tobin.
A person’s overall health plays a key role as well. When sick with something like the flu, there is already inflammation in the airway, nose and throat. This allows a person to absorb and process more of the protein that they’re allergic to, causing a more severe reaction. Environment is hugely influential also. And in Chicago, there are some disadvantages.
“Certainly, the pollution is a factor. It has been shown that [pollution], especially diesel fumes, exacerbate the allergic reaction,” says Tobin. “Many of my patients will tell me that they’ll have been in Wisconsin for the weekend, or they’ve been out of the Chicago area. And they can tell that they’re exposed to many of the same allergens, whether it’s tree or grass pollen, but as soon as they get back into the Chicago air, their symptoms worsen.”
But it’s not just pollen in the air that poses a potential threat to people trying to make the most of the good weather. In some cases, exercise can actually induce an allergic reaction called cholinergic urticaria, or exercise-induced hives.
“It’s estimated that one in 12 people will get hives at one time or another in their life,” says Dr. Paul A. Greenberger, professor of medicine, Division of Allergy-Immunology at Northwestern University Feinberg School of Medicine. Hives are often a reaction to food or medicine, to which the solution is simple; remove that food or medication from the equation.
Cholinergic urticaria (hives) can be vexing for people who are looking for that outside trigger and fail to realize that “the heating up of the body, by even one degree Fahrenheit, can result in a tendency to have itching on the body and then hives,” according to Greenberger. “If people are going to start running outdoors and they have this condition, they could pretreat with an antihistamine such as cetirizine. It’s sold without prescription.”
A more serious threat to completing that morning jog is a condition known as exercise-induced anaphylaxis. More rare, this condition can be life threatening. Anaphylaxis causes tightening of the airways, swelling, itching and can lead to loss of consciousness, amoung other symptoms. People may be familiar with the severe anaphylactic reaction caused by food, like peanuts or hypersensitivity to bee stings.
Greenberger explains that in the case of exercise-induced anaphylaxis, a foreign agent is not responsible. Rather “the exercise itself triggers or activates mast cells, which release their powerful contents. Histamine is one of them, but others include leukotrienes, prostaglandins and kinins. Kinins dilate blood vessels, which decrease the blood pressure and can put a person into shock.”
If you are experiencing an anaphylactic attack for the first time, you will need to get emergency care, but once aware of the condition, trips to the ER can be avoided. “Once the diagnosis is made, the patient can be given a plan to put into place,” says Greenberger. This plan would involve always carrying an Epi-Pen, an emergency tool for self-injecting the drug epinephrine, having a workout buddy and “learning that as soon as somebody starts having itching, they have to stop running or working out. That’s a hard one because people want to keep exercising,” says Greenberger.
If you’re having chronic allergic symptoms, it’s important to see a doctor who specializes in allergy treatment. Tobin says that people suffering from allergies “usually feel chronically crummy. And they don’t have to feel chronically crummy. If their allergies are under good control, they can really stay [as healthy as] most people.”
“We don’t have a cure [for allergies], Greenberger says. “We do have an approach; a treatment.”
—————————————————————————————————————————–
FOR MORE INFORMATION
Visit the website of the American Academy of Allergy, Asthma & Immunology at aaaai.org for useful information. For more information and help in finding a physician at Rush University Medical Center, visit rush.edu, and for more on Northwestern Memorial Hospital, visit nmh.org.