Covid-19 has caused a dramatic shift in organ transplants, with rising demand and more complex surgeries — all to prolong lives
Al Brown lay in a hospital bed at the Center for Care & Discovery at the University of Chicago Medicine, in disbelief. He had contracted Covid-19 in May 2020, during the early days of the pandemic. He knew the infection was serious, but he had no idea it would ravage his heart.
Initially, the Riverdale resident thought he had the flu and found it hard to breathe. He took himself to UChicago Medicine Ingalls Memorial Hospital in Harvey. Doctors there told him he had Covid-19. He was in the hospital for a week, hooked up to oxygen to help his breathing. Then he went back home, figuring he would recover.
But that recovery didn’t happen. A month later, every part of Brown’s body felt tired. He felt bloated. His corneas turned bloodshot and yellow. Everything he ate, he threw up. He could barely move.
He went back to Ingalls, where a new diagnosis stunned him: congestive heart failure — at age 30. Prior to this, Brown had no underlying medical conditions. He had lifted weights, run, and played with his two daughters.
On hearing the news, Brown sought a second opinion and was admitted to UChicago Medicine in Hyde Park in September 2020. A cardiologist told him his medications weren’t working and that his heart was functioning at 10% of its capacity.
“I was shocked,” Brown says. “My life kind of flashed before my eyes. Just like, what’s next?”
Over the phone, Brown told his daughters Naja and Akirah — who were then 10 and 6 — how sick he was and that he would need to stay in the hospital for a long time. Akirah cried so hard she needed to give the phone back to her older sister.
Doctors gave Brown a list of options, including implanting a pacemaker or a left ventricular assist device, which is a mechanical pump that helps the heart function. At the bottom of the list was a heart transplant.
Brown knew he didn’t want an artificial device implanted in his chest. He didn’t want multiple surgeries. He wanted a solution that would return him as close to his pre-Covid state as possible.
He took a few days to discuss his options with medical experts, family, and friends — over FaceTime, due to Covid restrictions at the time — and opted for a heart transplant.
Cases like Brown’s represent a dramatic shift. Covid-related emergencies have caused a rise in organ transplants — specifically lung transplants and to a lesser extent heart transplants.
Covid-19 can cause an outsized inflammatory response. The infection can severely damage air sacs that line the lungs. Fluid can then build up in the lungs, limiting the body’s ability to take in oxygen. Inflammation can also damage blood vessels and heart tissue, making the heart work harder to pump blood throughout the body.
In the most severe cases, Covid-19 damages the lungs and heart beyond recovery so that the only hope lies in expensive and drastic lung and heart transplants.
Lung troubles
A healthy 56-year-old from Sandwich, Illinois, Henry Garza had no underlying conditions before contracting Covid-19.
The week before Thanksgiving in 2020, Garza began to feel ill, bothered by a headache, cough, and fever. Every time he tried to get up, his body ached.
“I’ve never experienced anything like that,” he says. “My whole body hurt, bad. That’s when I realized, ‘Oh, I’m in trouble.’” Two days after the symptoms cropped up, he tested positive for Covid-19.
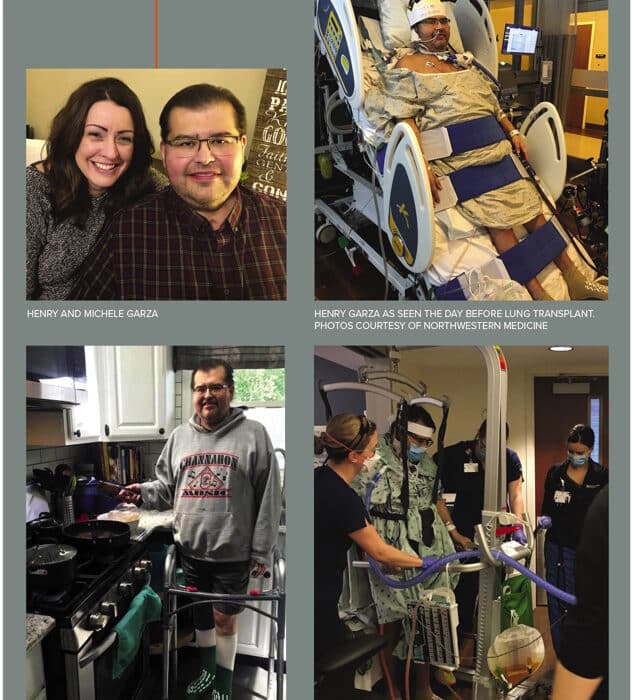
Within a few hours, doctors realized Garza needed more extensive care and transferred him to Northwestern Medicine Kishwaukee Hospital in DeKalb. He stayed there for the next month.
His symptoms didn’t improve. When he tried to stand, Garza gasped for air.
His doctors transferred him to Northwestern Memorial Hospital in Chicago so he could be hooked up to extracorporeal membrane oxygenation, or an ECMO machine. The ECMO essentially acted as his heart and lungs. Blood flowed out of Garza’s body and into the ECMO machine, which added oxygen, removed carbon dioxide, and warmed his blood before sending it back into his body.
ECMO is the highest level of heart- lung support a patient can receive, and the chances of lung recovery go down the longer an individual is dependent on the machine, says Garza’s surgeon, Ankit Bharat, MD, chief of thoracic surgery and executive director of the Canning Thoracic Institute at Northwestern Memorial Hospital.
People with Covid-19 who have been on ECMO for 40 days have a 5% chance of lung recovery, Bharat says. In total, Garza would be on ECMO for 116 days. His lungs were wrecked.
In January 2021, doctors told Garza that a double lung transplant would be his best option. By then, he says he had surrendered his care to God.
“There was just no turning around. The transplant had to happen.”
With tubes sprouting from his mouth and throat, he couldn’t speak. He spent hours each day lying prone — sometimes referred to as the “swimmer’s position,” face-down — to ease his breathing. His wife, Michele, FaceTimed him every night. She read to him, and she prayed with him.
In his head, Garza says he had continuous conversations with God, telling God that “if your plan is to take me home back to Michele and my family, then I know you’re gonna open the right doors and put the right doctors in place. If your plan is to take me home to you, then I’m not afraid.”
Garza says those conversations with God brought him great peace and comfort, especially when doctors told him he needed a transplant.
“My lungs, they just weren’t coming back,” he says. “Between battling the Covid-19 pneumonia, bacterial pneumonia, and different infections that I had throughout the hospital stay, there was just no turning around. The transplant had to happen. If I refused the transplant, you and I wouldn’t be talking right now.”
Increasing need for transplants
The demand for Covid-related organ transplants can be quantified in numbers. In 2020, Northwestern Memorial Hospital became the first hospital in the United States to perform a double lung transplant on a person with Covid-19. That year, Northwestern had 49 lung transplants, according to the Organ Procurement and Transplantation Network. Six of those were for Covid patients, the hospital says.
Demand quickly rose. In 2021, as Covid-19 continued to spread, the hospital performed 72 lung transplants. About 35 of those were double lung transplants due to Covid-19.
Those lung transplants have been a success. People with Covid-19 who had lung transplants from January 2020 to September 2021 have had a 100% survival rate so far, according to a study published in January 2022 in JAMA.
Nationwide, one in 10 lung transplants now go to people with Covid-19, according to data from the United Network for Organ Sharing.
Lung transplants are typically complex, but they are even more complicated in individuals with Covid-19. Unlike individuals with chronic pulmonary disease, like emphysema or cystic fibrosis, people with Covid-19 go into transplant surgery in much sicker states. Instead of walking into surgery, they’ve often been hooked up to an ECMO machine and a ventilator for months, as Garza was.
And while a double lung transplant for someone with chronic lung disease could take five to six hours, the same surgery for people with Covid-19 runs about 10 hours.

“It’s quite different than the standard lung transplants that we perform,” he says. “We have to learn how to deal with some of the immunological challenges that we see in these patients and how we manage them after the transplant.”
Challenges abound. People with Covid-19 may take medications and plasma therapy that make their immune systems more likely to reject newly transplanted lungs, Bharat says. So, while all transplant recipients require lifelong immunosuppressive drugs to prevent organ rejection, people with Covid require increased amounts, as well as other therapies.
The need for heart transplants due to Covid-19 hasn’t been as high as for lungs, but the virus has still caused an uptick, says Valluvan Jeevanandam, MD, chief of cardiac surgery at UChicago Medicine and director of its Heart and Vascular Center.
Organ transplants are expensive. Milliman, an actuarial and consulting firm, projected average total billed charges in 2020 for a lung transplant at $1.3 million and for a heart transplant at $1.7 million.
For older patients, Medicare usually covers heart and lung transplants (as well as kidney, pancreas, and liver transplants) for eligible individuals, but people with Medicare still need to pay a deductible and a 20% co-pay for outpatient expenses and drugs, among other costs. Supplemental insurance may help cover some of the remaining charges.
Waiting time for organ transplants
Nationally, people wait several months or longer for a lung or heart transplant. But the wait time is based on severity. And Covid-19 can cause severe damage.
Because of that severity, the wait time for a new lung or heart due to Covid-19 tends to be shorter than for someone with chronic disease. While the average list time at Northwestern for a lung transplant is 15 days, the average wait time for a Covid-related lung transplant is 11 days, Bharat says.
After doctors informed Garza in January 2021 that a double lung transplant would give him the best shot at survival, he joined the candidate waiting list with the Organ Procurement and Transplant Network, run by the U.S. Department of Health and Human Services.
Just two days after he joined the list, Garza’s care team told him they had found him a pair of lungs. But then, as they were preparing the donor lungs for Garza, they discovered a problem: The lungs had multiple blood clots and couldn’t be used.
Then, some more setbacks. Garza contracted a lung infection, which meant he couldn’t be relisted for transplant for a few more weeks.
“It felt like a year because you just don’t know if it’s going to happen,” Garza says. “I asked one of the physician assistants, ‘At one point, do you just give up on me? Do you just throw your hands up and say, “We can’t find your lungs. We can’t do this anymore”?’ He almost kind of laughed, and he’s like, ‘No, we’ll never give up.’”
Finally, around 4:30 p.m. on April 14 — after four months of being hooked up to an ECMO machine — doctors told Garza they had matched him with a pair of problem-free donor lungs. He would go into surgery to receive them that night.
Things moved much faster for Al Brown’s heart transplant.
Brown had signed all the transplant paperwork and was listed in early October 2020. Within two weeks, he got a call: A donor heart was ready. Just before 10 a.m. that day, the transplant team wheeled Brown into surgery.
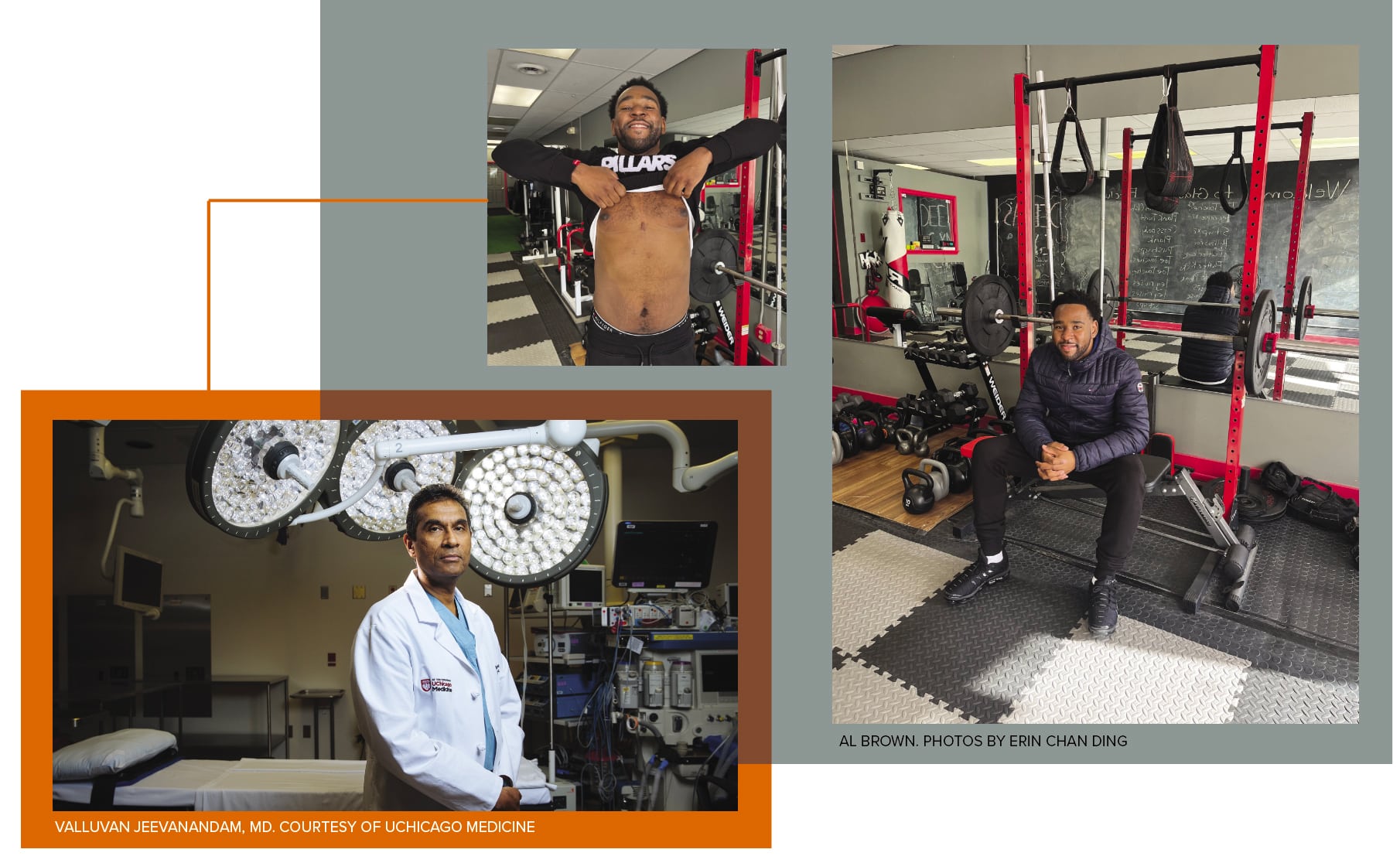
A heart typically needs to be out of a donor and into the recipient within four hours, but if necessary, UChicago uses techniques to stretch that time to about five and a half hours, Jeevanandam says. The transplant surgeries themselves can range from five to 16 hours.
After Brown’s transplant, doctors and nurses told him that he woke up the following day and flitted in and out of consciousness. He doesn’t remember any of it. The next thing he recalls, it was three days later, and he realized he had a new heart.
Freedom and gratitude
For Brown and Garza, the organ transplants meant not only survival but freedom. The heart transplant untethered Brown from a balloon pump that constantly hissed as it distributed blood to his body.
Garza’s double lung transplant liberated him from a bevy of machines. Three days after his transplant, doctors removed Garza from his ECMO machine. Five days later, Garza came off of his ventilator, and the day after that, hospital staff removed his tracheostomy tube.
“It was incredible for many reasons,” he says. “You’re not tethered down. It’s just a great feeling of being free.”
Garza remembers the first meal he ate nine days after his double lung transplant: chicken broth, Jell-O, and lemonade. For the first time in the four months since he had been put on a ventilator, he ingested food via his mouth instead of through a nasogastric tube.
“I’ll tell you what, that was the best chicken broth I’ve ever had,” he says, laughing.
Garza stayed in the hospital for three weeks after his transplant and then transferred to Shirley Ryan AbilityLab for intense physical therapy. He stayed there for another month before his next-door neighbors in Sandwich threw a street party to welcome him home.
Brown also stayed in the hospital for another month to recover from his transplant. During that time, he relearned how to walk.
When he finally came home to south suburban Riverdale, he was able to feel his pulse on his wrist, something he could not do when his old heart had been failing.
Brown said his daughters looked shocked to see him. For the first time in three months, he wrapped his arms around them. His youngest daughter, Akirah, erupted into tears. So did Brown.
Brown, now 32, talks as he sits on an exercise bench at Gladiator Fit Club, his cousin’s CrossFit gym in south suburban Lansing. After his discharge, he went to cardiac rehabilitation three times a week for three months. He exercises now to keep his heart strong.
His current workout routine includes five-mile treadmill runs three days a week, kettle bells, push-ups, pull-ups, and deadlifts. There’s no physical evidence of his transplant until he pulls up a black T-shirt to reveal a three-inch scar atop his sternum.
Brown says he’s thankful now, for everything. “I am thankful and grateful for everything. The stuff that I would complain about before, I would never complain about now. I feel that my life has been blessed,” he says.
Garza, in fall 2021, walked an entire mile. His family took photos. About a month later, he made it two miles. Someday, he says, he wants to run the Bank of America Chicago Marathon.
For now, Garza takes a daily cocktail of 27 pills to prevent infection and organ rejection. Like Brown, he’ll be on medication for the rest of his life, but to Garza, it’s well worth the tradeoff.
“I think about it, and it’s like, ‘Man, I’m still alive because of these lungs,’” Garza says.
Increasing Transplant Access Across Racial Lines
During her residency a decade ago, Dinee Simpson, MD, was participating in a rotation in the transplant service when she noticed something: All six patients being evaluated for a kidney transplant in the clinic that day were Black.
Simpson, now a transplant surgeon at Northwestern Medicine, consulted medical research and found that Black patients were four times more likely to develop kidney disease than white patients.

The vast majority of the time, the causes are not genetic, she says. The disparities often correlate with social determinants of health and access to care.
“It’s related to structured environment,” says Simpson, vice chair for faculty development and diversity in the department of surgery at Northwestern University Feinberg School of Medicine. “It’s related to institutional barriers that exist, implicit biases that exist. And so that was really profound to me.”
Simpson, who is Black, noticed something else: The Black patients had an emotional reaction upon seeing her walk into a room wearing her lab coat. She was the first Black doctor some of them had seen.
“They told me they felt like they could trust me. They felt like they might have a better chance at making it through the transplant process, just because I was involved,” she says.
Simpson would go on to become a kidney and liver transplant surgeon. In 2018, Northwestern Medicine hired her to launch the country’s first African American Transplant Access Program, or AATAP. By the end of 2021, Simpson says 19 patients had received organ transplants through the program.
The program is built specifically to help Black people navigate complicated transplants and a complex healthcare system. Simpson starts by building trust — often fractured because of a legacy of racism in healthcare, along with lower-quality services and experimental procedures.
Simpson, who evaluates every potential transplant recipient, works with a social worker, a health literacy coach, a psychiatrist, and a nurse coordinator. Together, they build relationships with patients and their families, keeping appointments patient-centered and open-ended to encourage people to feel comfortable and informed about the transplant process.
The team also connects families with resources such as insurance assistance, transportation assistance, and support groups.
“A lot of those barriers [to organ transplantation] are modifiable,” Simpson says. “So that’s what the program is designed to do: Pick out a handful of things where we, as an institution, can make a difference.”













