Your neural networks have a lot to say — and bioelectronic medicine might help you listen
Imagine putting on an adhesive bandage. Now imagine that bandage could continuously monitor your vital neural functions to catch signs of illness before they become problematic. Even further, imagine that bandage could actually prevent illness from occurring and help you heal faster when it does.
This is the promise of bioelectronic medicine, a growing field of study exploring how to monitor, diagnose and treat individuals using noninvasive, skinlike wearables and injectable devices that biodegrade safely in your body.
John Rogers, PhD, is a physical chemist and the founder and director of the Center for Bio-Integrated Electronics at Northwestern University. He’s also one of the foremost scientists working on developing biocompatible medical devices that can seamlessly integrate with the human body to collect physiological data and promote healing in truly profound ways.
“We’ve done a lot of work on devices that interface to the skin, brain, heart, bladder, spinal cord and peripheral nervous system — all of these different soft tissue systems where electronic sensing and stimulation can improve organ function and provide deep insights into physiological health,” Rogers says. “It’s all geared toward making healthcare more effective and less costly.”
The science of bioelectronic medicine
To understand how these devices work, Rogers says, think of consumer gadgetry already in mainstream use — things like radios, microprocessors and Bluetooth devices. Bioelectronic medicine takes these same standard electronic processes and applies them to devices with the soft textured surfaces of the vital organs of the human body. These skinlike electronics have thin membranes that laminate onto biological tissues in a minimally invasive and biocompatible manner. Once activated, they integrate seamlessly with the body’s organs for diagnostic and therapeutic use.
“You have twin technology development streams — one is software and data analysis, and the other is skin interface soft body electronics,” Rogers says. When these streams converge, you get devices that can monitor an individual’s health accurately and continuously and share that data with physicians.
“The goal is to bring clinical-grade measurement technology out of the clinic and into the wild — at the home and the workplace and so on — so you’re not confined to just episodic measurements of physiological health,” Rogers says.
Bringing bioelectronic devices mainstream
Bioelectronic devices have been about a decade in the making, but don’t expect to see many in use just yet. Collecting and sharing insights about neural networks in real time raises a few questions, most notably about data security and how to regulate access to the information that’s gathered. And those kinks will have to be worked out first.
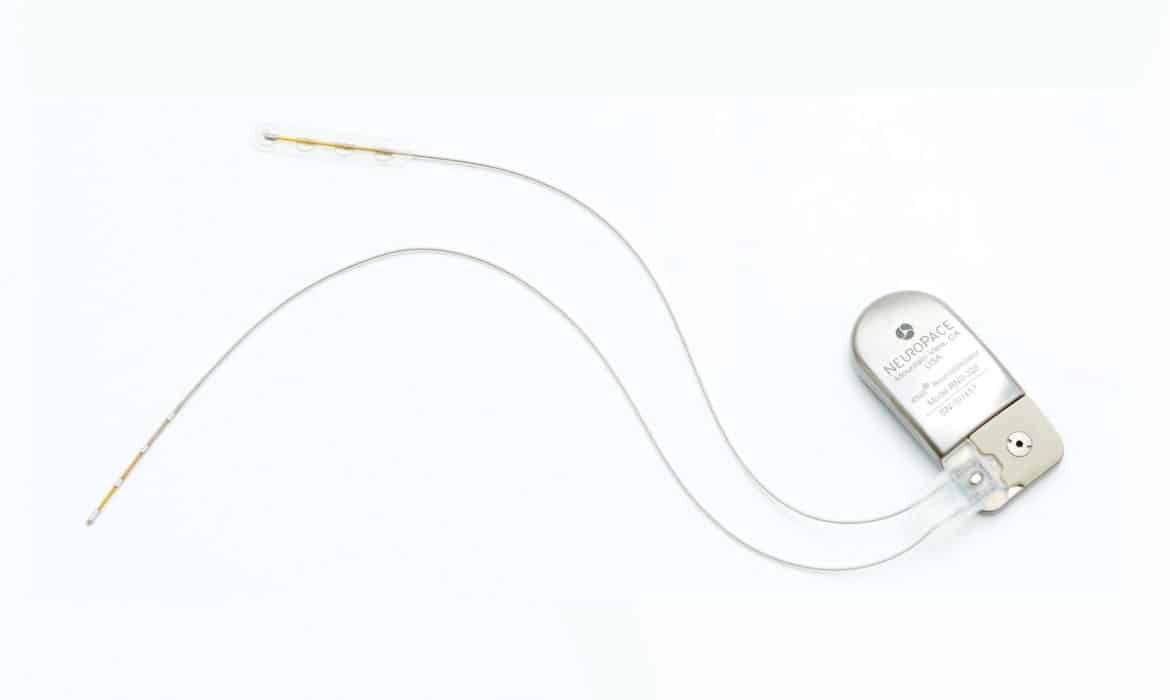
The promises of bioelectronic medicine aren’t all in the future, though. At NorthShore University HealthSystem’s pediatric neurology and epilepsy program, physicians are using NeuroPace, the first neural modulator device available for monitoring and preventing seizure activity.
“This implanted device uses bioelectronic medicine to monitor, detect and record neural activity,” says pediatric neurologist Takijah Heard, MD,who uses NeuroPace to treat her patientswith epilepsy. “It then detects the pattern that leads to seizure and delivers a dose of energy to cancel out the abnormal electrical activity coming from the brain,” thereby aborting the seizure.
And at Northwestern, about 10,000 neural devices created at the Center for Bio-Integrated Electronics are being sent to India, Pakistan, Zambia and Kenya as part of a partnership with the Bill & Melinda Gates Foundation and Save the Children to provide widespread bioelectronic monitoring of maternal, fetal and neonatal health.
Looking forward, Rogers envisions the mass production of bioelectronic devices for consumer benefit and a future for healthcare that’s no longer confined to the doctor’s office.